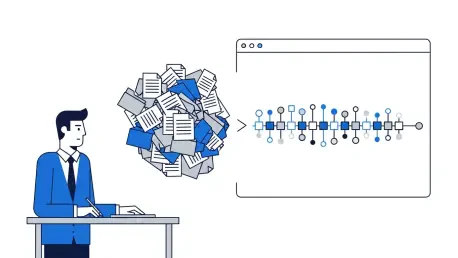
The modern insurance claims process is governed by a relentless influx of information, where adjusters are tasked with navigating a digital deluge of reports, invoices, estimates, and correspondence that arrives through countless channels. This constant stream of unstructured data creates a significant operational chokepoint, forcing highly skilled professionals to spend an inordinate amount of their time on low-value administrative tasks like sorting, classifying, and manually keying in information. This document bottleneck not only slows down the entire claims lifecycle, leading to frustrated policyholders and increased operational costs, but it also diverts the attention of adjusters away from their most critical functions: investigating complex claims, making informed decisions, and providing empathetic support to customers during their time of need. As the volume and velocity of data continue to grow, the pressure on claims departments to find a more efficient path forward has become more intense than ever, pushing the industry toward a technological tipping point.
The Advent of Intelligent Automation
To counteract this pervasive inefficiency, the industry is now turning to a new generation of intelligent automation powered by artificial intelligence. These advanced systems function as sophisticated AI agents integrated directly within core claims management platforms, such as Guidewire ClaimCenter. Operating around the clock, these agents continuously monitor all document intake channels, from emails to customer portals, to intercept incoming files before they ever reach a human queue. Leveraging advanced machine learning models trained specifically on insurance-related documents, the technology can automatically classify an extensive array of file types with remarkable precision. With the ability to distinguish between more than 70 different document categories, including medical records, police reports, and repair invoices, these AI agents are achieving accuracy rates that exceed 98%. This level of automation can effectively handle up to 90% of all incoming documents, transforming a traditionally manual and error-prone process into a streamlined, touchless workflow.
The true power of this technology extends far beyond simple sorting and classification, however. Once a document has been correctly identified, the AI agent employs sophisticated data extraction capabilities to read and comprehend the information contained within it. It intelligently identifies and pulls key data points—such as dates of service, policy numbers, claimant names, and total amounts—and automatically inputs this information into the correct fields within the claims file. This eliminates the tedious and redundant task of manual data entry, a major source of both delays and human error. By bridging the gap between unstructured documents and structured system data, these agents enable a much higher degree of straight-through processing. The result is a claims file that is populated with accurate, relevant information almost instantaneously, allowing human adjusters to begin their substantive work with a complete and organized record from the very start of the process.
Redefining the Claims Operation
The implementation of such a high degree of automation delivers profound and measurable benefits for insurers. By drastically reducing the need for manual intervention in document handling, carriers can significantly shorten overall claim cycle times, a key metric for both operational efficiency and customer satisfaction. The elimination of redundant document reviews and manual data entry directly translates into lower operational expenses, as it reduces the reliance on costly third-party processing services and frees up internal resources. Consequently, insurers are better positioned to deliver faster claim payments, which not only improves the policyholder experience but also serves as a powerful competitive differentiator in a crowded market. The system fosters a more consistent and high-quality customer journey by ensuring that every claim file is handled with the same speed and accuracy, minimizing the variability that often accompanies manual processing and creating a more predictable and reliable service environment.
A Fundamental Shift in Focus
Ultimately, the integration of advanced AI into core claims systems represented a pivotal step in modernizing legacy insurance processes. The seamless availability of these tools within established platforms ensured that implementation was streamlined and rapid, allowing carriers to realize significant improvements in performance without disrupting their existing infrastructure. This technological advancement did more than just accelerate a workflow; it fundamentally redefined the role of the claims adjuster. By offloading the burden of routine administrative work, the technology empowered adjusters to dedicate their expertise to higher-value activities. They were able to concentrate on making critical coverage decisions, negotiating complex settlements, and, most importantly, engaging directly with customers to provide guidance and support. This shift transformed the claims department from a processing center into a hub of strategic decision-making and customer advocacy, proving that the greatest value of automation was not just in the tasks it completed, but in the human potential it unlocked.