As we dive into the evolving world of insurance technology, I’m thrilled to sit down with Simon Glairy, a renowned expert in insurance and Insurtech, with deep expertise in risk management and AI-driven risk assessment. Today, we’re exploring a groundbreaking development in claims management through Simon’s insights on innovative platforms that leverage AI to transform how claims are handled. Our conversation touches on the inspiration behind such tools, the role of advanced technology in enhancing client outcomes, the importance of transparency, and the global strategy for implementing these solutions.
How did the idea for an AI-driven claims management platform come about, and what challenges were you aiming to address?
The concept stemmed from a clear need in the industry to streamline claims processes and improve outcomes for clients. We saw persistent issues like inconsistent handling across regions, delays in resolution, and a lack of actionable insights for both clients and professionals. The goal was to create a tool that not only automates mundane tasks but also empowers our teams with data to advocate more effectively. It was about bridging the gap between complex claims and faster, fairer resolutions while ensuring clients felt supported every step of the way.
Can you walk us through what an AI-enabled claims platform entails and how it benefits clients in practical terms?
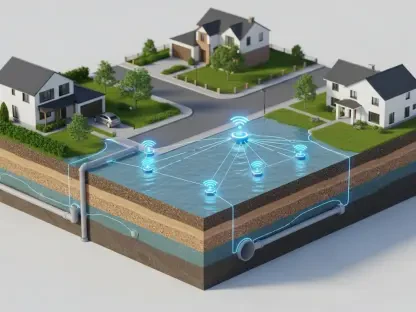
At its core, it’s a digital hub that manages every phase of a claim—from initial intake to final resolution. It integrates automation for routine tasks like documentation and uses AI to analyze data for smarter decision-making. For clients, this means faster processing times and a clearer picture of their claim’s progress through accessible portals. Compared to traditional methods, it cuts down on manual errors and speeds up communication, so clients aren’t left waiting for updates or outcomes.
In what ways does AI technology specifically enhance the claims process within such a platform?
AI plays a pivotal role by sifting through massive amounts of data to identify patterns and predict outcomes. It pulls insights from historical claims, market trends, and even specific carrier performance to guide decisions. This also ensures consistency across different countries by standardizing processes while still adapting to local nuances. The result is a more reliable and efficient system where decisions aren’t just reactive but proactive, anticipating issues before they escalate.
What are some of the key features of these platforms that stand out for both clients and claims professionals?
For clients, real-time dashboards are a game-changer. They can see trends in their claims, understand portfolio performance, and gauge how quickly issues are resolved. For our teams, automation of tasks like claim intake frees up time to focus on advocacy. Plus, the analytics help us build stronger cases by providing hard data to support negotiations. It’s about giving everyone—clients and professionals—tools to work smarter, not harder.
How does a platform like this evaluate the performance of insurance carriers, and why does that matter to clients?
It tracks specific metrics like how fast carriers close claims, the efficiency of their processes, and the quality of their outcomes. This data creates a feedback loop that helps us identify which carriers consistently deliver. For clients, this is crucial because it informs decisions on who to partner with for coverage. Knowing which carriers perform best under pressure ensures their risks are managed by reliable hands, ultimately protecting their interests.
Can you explain how these platforms improve transparency for clients during the claims process?
Transparency is built into the design with dedicated client portals. Clients can log in anytime to track their claim’s status, view updates, and access relevant documents. This level of visibility gives them a sense of control—they’re not left in the dark waiting for phone calls or emails. It builds trust, as they can see exactly where things stand and feel confident that their concerns are being addressed in real time.
How does this kind of technology support claims professionals in their daily work and advocacy efforts?
It’s a huge boost for our teams. The platform provides tools to prepare complex claims with data-backed arguments, making presentations to carriers or other stakeholders more compelling. It also streamlines workflows, so professionals can focus on strategy rather than paperwork. This enhances their ability to push for maximum recoveries and shortens the claim lifecycle, ensuring clients get the best possible outcome without unnecessary delays.
What factors influence the decision to launch such a platform in a specific country first, and how is the global rollout planned?
Choosing an initial launch location often depends on market readiness, regulatory environment, and client demand. For instance, a country with a high concentration of commercial clients or unique risk challenges might be prioritized to test and refine the platform. The global rollout is typically phased to ensure we adapt to regional needs, with timelines set to gradually cover more territories over a couple of years. It’s a balance of learning from early deployments and scaling with precision.
What is your forecast for the future of AI in claims management and its impact on the insurance industry?
I believe AI will become the backbone of claims management in the next decade. We’re just scratching the surface with automation and analytics—future advancements will likely include even more predictive capabilities, perhaps anticipating claims before they’re even filed. This could revolutionize risk mitigation and pricing models. For the industry, it means greater efficiency and client satisfaction, but it’ll also demand a shift in skills, with professionals needing to adapt to tech-driven workflows. It’s an exciting, transformative road ahead.