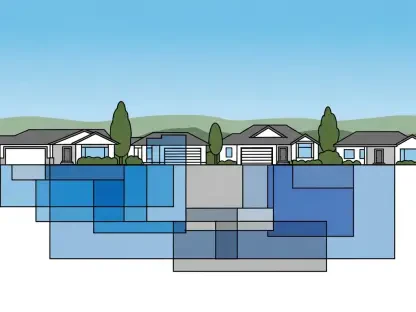
In a groundbreaking development that could reshape the landscape of healthcare for millions of Americans, the Trump administration has rolled out a pilot program named WISeR (Wasteful and Inappropriate Service Reduction), which integrates artificial intelligence (AI) into the decision-making process for Medicare treatment approvals. Launched this year, the initiative targets wasteful spending and fraud within Medicare, the federal health insurance program serving seniors and certain individuals with disabilities. Running through 2031, the program deploys AI algorithms across six states—Arizona, Ohio, Oklahoma, New Jersey, Texas, and Washington—to assess the necessity of specific medical services. This marks a historic shift for traditional Medicare, which has long avoided the stringent prior authorization measures common in private insurance. The initial focus includes treatments like skin substitutes, nerve stimulator implants, and knee arthroscopy, with potential expansion to other procedures. While the stated aim is to enhance efficiency and curb costs, this move has ignited intense debate over access to care, patient outcomes, and the ethical implications of entrusting such critical decisions to technology. The promise of streamlined processes stands in stark contrast to fears of automated denials that could jeopardize necessary care, setting the stage for a contentious rollout as stakeholders grapple with the balance between innovation and patient well-being.
Transforming Medicare with AI-Driven Decisions
The WISeR pilot introduces a profound change in how traditional Medicare operates by incorporating prior authorization—a process requiring pre-approval for certain treatments—on a broader scale than ever before. Unlike Medicare Advantage plans or private insurers, where this practice is routine, traditional Medicare has historically minimized such barriers to care. Now, with AI at the helm in the selected states, the program seeks to identify and deny “low-value” services deemed unnecessary by algorithmic analysis. The Centers for Medicare & Medicaid Services (CMS) champions this approach as a way to reduce human error and save taxpayer dollars by targeting fraud and overuse. However, the shift raises significant questions about whether a system designed for efficiency can adequately address the complex, individual needs of patients. Concerns linger over the potential for technology to overshadow clinical expertise, especially when the stakes involve life-altering medical interventions. As the pilot unfolds, its impact on care delivery in these six states will serve as a critical test of whether AI can be a tool for progress or a source of new obstacles in an already burdened healthcare system.
Beyond the technological innovation, the WISeR initiative reveals deeper tensions about the direction of Medicare policy. Critics argue that adopting prior authorization mirrors private insurance strategies often criticized for placing financial savings above patient health. The fear is that algorithms, no matter how advanced, might lack the nuance to interpret unique medical histories or rare conditions, leading to denials that could delay vital treatments. CMS has pledged that human clinicians will review AI decisions to prevent such outcomes, yet doubts persist about the thoroughness of these safeguards. Reports from private insurance, where AI has sometimes resulted in hasty or erroneous denials, fuel skepticism about whether similar issues could emerge in Medicare. The definition of “low-value” care itself remains contentious, as what may seem unnecessary to an algorithm could be essential to a patient’s quality of life. This pilot, therefore, is not just a technological experiment but a litmus test for how far cost-control measures can extend before they infringe on the fundamental promise of accessible healthcare for Medicare beneficiaries.
Public and Professional Resistance to Automated Approvals
Public sentiment toward prior authorization, even before the advent of AI, has long been marked by frustration, and the WISeR pilot has only intensified this discontent. A recent poll by KFF found that nearly 75% of Americans consider prior authorization a major barrier to care, citing delays and denials that often lead to worsened health outcomes. Patients frequently share stories of waiting weeks for approvals, only to face rejections that force them to forgo necessary treatments or incur significant out-of-pocket costs. With AI now entering the equation, there’s a palpable fear that automation could exacerbate these issues, turning a flawed process into an even more impersonal and rigid system. The emotional toll of navigating such hurdles, especially for vulnerable populations like seniors, cannot be overstated, as delays in care can mean the difference between recovery and irreversible harm. This widespread dissatisfaction sets a challenging backdrop for the pilot, as public trust in Medicare’s ability to prioritize patient needs over fiscal goals hangs in the balance.
Healthcare professionals echo these concerns, with many expressing alarm at the prospect of AI overriding clinical judgment. Surveys conducted by the American Medical Association reveal deep unease among physicians, who fear that denial rates could spike under automated systems, creating additional administrative burdens and compromising patient safety. Doctors argue that algorithms cannot replicate the nuanced decision-making that comes from years of medical training and direct patient interaction. High-profile incidents of public outrage over insurance denials in recent years further amplify these worries, as they highlight the human cost of bureaucratic barriers to care. For the WISeR pilot, this professional backlash poses a significant hurdle, as providers may resist a system they perceive as undermining their autonomy and the well-being of those they serve. The tension between technological efficiency and the human element of medicine remains a core issue, with many in the field calling for robust oversight to ensure that patient care isn’t sacrificed for the sake of cost savings.
Policy Contradictions and Political Pushback
The rollout of the WISeR pilot has been clouded by apparent contradictions in the Trump administration’s stance on prior authorization. Just days before unveiling this AI-driven initiative, the administration introduced a voluntary effort with private insurers to streamline and reduce prior authorization, acknowledging its detrimental effects on care delivery and public trust. This dual messaging has drawn sharp criticism from lawmakers and policy experts, who question why Medicare is expanding a practice that the government itself has critiqued in the private sector. Such inconsistency fuels accusations that fiscal priorities are trumping patient advocacy, casting doubt on the sincerity of broader healthcare reform efforts. The discrepancy has not only confused stakeholders but also eroded confidence in the pilot’s intentions, as many wonder whether the focus is truly on improving outcomes or merely cutting costs at any expense. This political misstep underscores the delicate balance required when introducing transformative policies in a system as critical as Medicare.
Bipartisan concern has emerged as a powerful force against the WISeR pilot, with legislators from both parties voicing reservations about its implications. Democrats have pressed for greater transparency and accountability, with some proposing to block funding for the program in upcoming budgets. Republicans, including those with medical backgrounds, have similarly cautioned against allowing AI to interfere with physicians’ decision-making authority, emphasizing the importance of preserving access to care. This rare cross-party alignment reflects a shared understanding that while innovation holds promise, it must not come at the cost of patient well-being. The political pushback signals a broader unease with untested technological interventions in healthcare, particularly within a program as vital as Medicare. As debates continue, the pilot faces scrutiny that could shape not only its trajectory but also the future of AI applications in federal health policy. The outcome of these discussions may well determine whether this initiative becomes a model for efficiency or a cautionary tale of overreach.
Weighing AI’s Potential Against Its Pitfalls
Advocates of the WISeR pilot highlight the potential benefits of AI in revolutionizing Medicare’s approach to resource allocation. CMS contends that algorithms can minimize bias, accelerate approval processes, and ensure that taxpayer funds are directed toward genuinely necessary treatments. By identifying fraudulent claims and curbing overuse, AI could save billions, proponents argue, while maintaining or even improving care quality through consistent decision-making. Safeguards such as mandatory human review of AI determinations are cited as evidence of a commitment to balance, with CMS asserting that clinicians will have the final say in contested cases. This optimistic view positions the pilot as a forward-thinking solution to longstanding inefficiencies, offering a glimpse into a future where technology enhances rather than hinders healthcare delivery. For supporters, the initiative represents a chance to modernize Medicare in a way that aligns with broader goals of fiscal responsibility and fraud prevention, provided that oversight remains robust.
Skeptics, however, caution against overreliance on AI, pointing to significant risks that could undermine the pilot’s objectives. Examples from private insurance, where automated systems have led to hasty denials and flawed outcomes, cast a shadow over claims of “meaningful human review.” Reports suggest that some reviews are perfunctory, lasting mere seconds, raising doubts about whether similar lapses could occur in Medicare. Additionally, the financial incentives for vendors managing the WISeR program draw scrutiny, as shared savings arrangements might encourage denials of medically necessary care to boost profits. Transparency in how algorithms are designed and operate remains a glaring gap, with experts warning that without clear accountability, patients could bear the brunt of errors through delayed treatments or unexpected costs. The challenge lies in ensuring that AI serves as a tool to support, rather than dictate, clinical decisions—a balance that has yet to be proven achievable as the pilot begins its multi-year run.
Navigating the Future of Healthcare Innovation
Reflecting on the launch of the WISeR pilot, it’s evident that this initiative has stirred a complex dialogue about the intersection of technology and healthcare. The program’s ambition to address waste and fraud in Medicare through AI was met with both cautious optimism and significant apprehension from various quarters. Public frustration, professional resistance, and political scrutiny underscored the deep-seated challenges of integrating automated systems into a domain as personal as medical care. While CMS maintained that safeguards were in place to protect patients, the specter of automated denials and insufficient oversight lingered as a persistent concern throughout the early discussions.
Looking ahead, the path forward demands actionable steps to ensure that innovation enhances rather than compromises patient outcomes. Rigorous evaluation of the pilot’s impact across the six participating states must be prioritized, with transparent reporting on denial rates, patient experiences, and cost savings. Strengthening human oversight through well-defined protocols could help mitigate the risks of algorithmic errors, while engaging healthcare providers in the design of AI tools might foster greater trust and efficacy. Policymakers should also consider legislative measures to enforce accountability among vendors, eliminating incentives that prioritize profit over care. As the program progresses through 2031, its lessons will likely inform broader applications of AI in healthcare, offering a critical opportunity to refine technology’s role in supporting, rather than supplanting, the human judgment at the heart of medicine.