In today’s complex landscape of workers’ compensation, a growing body of evidence points to social determinants of health (SDOH) as pivotal factors driving up costs and delaying recovery for injured employees. These non-medical elements—ranging from income levels and housing stability to education and access to social support—profoundly shape how individuals navigate the recovery process after workplace injuries. Far beyond the scope of traditional medical treatment, these external conditions often dictate whether a worker returns to their job swiftly or faces prolonged disability, ultimately inflating claim expenses for insurers and employers. This article explores the intricate ways in which social and environmental barriers contribute to escalating costs, examines real-world implications, and highlights innovative strategies that the industry is adopting to address these challenges. By shedding light on this often-overlooked aspect of claims management, a clearer path emerges for improving outcomes and controlling financial burdens.
Unpacking the Rising Costs of Claims
The Burden of Complex Cases
Over the past two decades, workers’ compensation claims have seen a steady rise in costs, with a significant portion of expenses tied to a small number of complex cases. These claims frequently involve not only physical injuries but also overlapping mental health challenges, creating a web of complications that extend recovery periods far beyond initial expectations. Despite representing just a fraction of total cases, their disproportionate impact on resources stems from prolonged disability durations and the need for extensive medical and legal interventions. This financial strain underscores a critical need to dig deeper into underlying causes, as simply addressing medical symptoms often fails to resolve the full scope of issues. Industry stakeholders are increasingly recognizing that without tackling these root factors, cost containment remains an elusive goal, pushing the need for a broader perspective on what influences recovery.
Social and Environmental Barriers at Play
A key driver behind these escalating costs lies in social and environmental barriers that hinder an injured worker’s ability to heal effectively. For example, a worker residing in a rural area may face significant obstacles in accessing specialized medical care due to long distances and limited transportation options, resulting in delayed treatments. Similarly, those without a strong family or community support system might struggle with basic daily tasks during recovery, further slowing their return to work. Such barriers, though unrelated to the injury itself, can transform a straightforward claim into a drawn-out ordeal with mounting expenses. These scenarios reveal how non-medical conditions often play a more decisive role than clinical factors in determining the trajectory of a claim, urging a shift in how the industry approaches case management to account for these external influences.
Understanding Social Determinants in Claims Management
The Hidden Drivers of Cost and Complexity
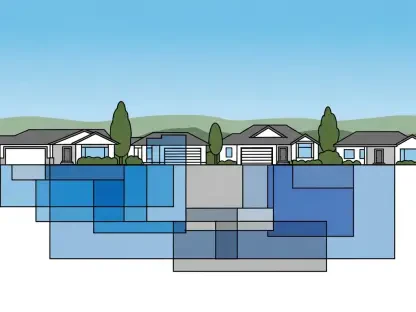
Social determinants of health, such as geographic isolation, financial instability, and inadequate social networks, often remain under the radar in traditional workers’ compensation strategies, yet their impact on costs is undeniable. A worker grappling with economic hardship may delay seeking follow-up care due to an inability to afford out-of-pocket expenses, leading to worsening conditions that require more intensive treatment later. Similarly, those in remote locations might miss critical appointments because of unreliable public transit, extending their time away from work. These factors directly correlate with longer disability periods and a higher likelihood of litigation, as unresolved issues compound over time. Recognizing these elements as central to claims outcomes rather than peripheral concerns is essential for insurers and employers aiming to curb financial losses while supporting injured workers more effectively.
Real-World Disparities in Recovery Outcomes
The tangible effects of social determinants become strikingly clear when comparing recovery outcomes among workers with similar injuries but different life circumstances. Consider two individuals with identical knee injuries: one has stable housing and a supportive family, enabling a swift return to modified duties, while the other faces financial stress and lacks reliable transportation, resulting in months of delayed recovery. Such disparities illustrate how external conditions can overshadow medical treatment in shaping the duration and cost of a claim. The worker without adequate resources often encounters cascading challenges, from missed therapy sessions to heightened mental strain, which further complicate the healing process. This stark contrast emphasizes the urgency of addressing non-medical factors as a core component of claims management to prevent unnecessary escalation of expenses and improve overall worker well-being.
Strategies to Mitigate SDOH Challenges
Early Intervention and Human Connection
One of the most effective ways to counteract the impact of social determinants on workers’ compensation costs is through early intervention that prioritizes identifying barriers immediately after an injury. Structured intake processes, often led by trained nurses or case managers, allow for the documentation of non-medical challenges—such as lack of childcare or transportation difficulties—during the initial assessment. By addressing these issues within the critical first month post-injury, potential delays can be minimized before they spiral into costly setbacks. This high-touch approach not only fosters trust between the injured worker and the claims team but also ensures that recovery plans are tailored to the individual’s unique context. Evidence suggests that such proactive engagement significantly shortens return-to-work timelines and reduces the likelihood of legal disputes, offering a dual benefit of cost savings and improved outcomes.
Technology as a Tool for Targeted Solutions
Complementing human intervention, technology plays a vital role in identifying and addressing social determinants that influence claims costs. Predictive analytics and dynamic risk-scoring tools enable claims teams to flag high-risk cases early, pinpointing workers who may face social or environmental hurdles that could derail recovery. For instance, algorithms can highlight a case where transportation barriers are likely to cause missed appointments, prompting case managers to arrange alternative solutions like virtual consultations or rideshare services. When paired with human judgment, these digital tools ensure a balanced response that allocates resources efficiently while maintaining a personal touch. This synergy between technology and empathy allows for customized interventions that tackle specific challenges, ultimately reducing the duration of disability and keeping expenses in check for insurers and employers alike.
Building a Holistic Approach
Person-Centered Recovery Plans
To truly address the impact of social determinants on workers’ compensation costs, a shift toward person-centered recovery plans is imperative. This approach goes beyond treating the injury itself by integrating comprehensive data on a worker’s medical history, psychosocial conditions, and environmental risks into the claims process. For example, understanding that a worker is a sole caregiver for dependents can prompt adjustments like flexible therapy schedules or home-based care options, preventing unnecessary delays in healing. Such tailored strategies not only enhance the individual’s well-being but also create predictability in cost management by avoiding complications that arise from unaddressed social barriers. By viewing the injured worker as a whole person rather than a collection of symptoms, claims management can achieve more sustainable outcomes that benefit all stakeholders involved.
Future Innovations in Claims Management
Looking ahead, the workers’ compensation industry stands on the brink of transformative change with emerging technologies like artificial intelligence (AI) offering new ways to address social determinants. AI has the potential to analyze vast datasets, including unstructured information from intake notes, to predict recovery obstacles tied to social factors with unprecedented accuracy. This capability could enable even earlier and more precise interventions, such as connecting workers to community resources before challenges escalate. While these advancements hold immense promise for refining risk models and enhancing outcomes, the irreplaceable value of human empathy remains a cornerstone of effective claims handling. As innovation continues to evolve, striking a balance between cutting-edge tools and compassionate care will be key to navigating the complexities of social determinants, ensuring that both financial and human costs are managed with foresight and sensitivity.