Imagine a scenario where a life-saving medical treatment is denied by an insurance provider, leaving a patient and their family in despair, grappling with the financial burden and emotional toll of such a decision, while countless individuals across the D.C. area, including Washington, D.C., Maryland, and Virginia, face this harsh reality far too often. Many remain unaware of a critical legal tool at their disposal: the external appeal process. This mechanism allows patients to challenge insurance denials through an independent review, potentially reversing decisions that could mean the difference between recovery and hardship. Despite protections bolstered by federal legislation like the Affordable Care Act, gaps in awareness and systemic barriers persist, often due to limited information and complex processes. This article explores how residents in the D.C. region can leverage external appeals to fight back against unfair denials, highlighting state-specific resources, actionable steps, and the urgent need for greater public knowledge to ensure access to necessary care.
1. Understanding the Power of External Appeals
External appeals represent a vital lifeline for patients whose insurance claims for essential treatments have been rejected, offering a chance to have decisions reviewed by independent experts outside the insurer’s influence. A compelling case uncovered by investigative reporting showcased a North Carolina couple, Teressa Sutton-Schulman and her husband, who battled repeated denials for psychiatric care following severe mental health crises. After navigating the cumbersome appeal process, an independent reviewer overturned the insurer’s decision, compelling coverage for over $70,000 in treatment costs. This example underscores the potential of external appeals to secure critical care when all seems lost. However, despite federal enhancements to appeal rights over a decade ago, many patients remain in the dark about this option. Insurance industry pushback has often diluted protections, resulting in unclear communication and restricted eligibility, leaving countless individuals without the knowledge or means to challenge unfair denials effectively.
The lack of awareness surrounding external appeals is a significant barrier, compounded by the emotional and physical exhaustion patients often face during serious health challenges. Many give up on pursuing their rights, not realizing that a successful appeal could dramatically alter their circumstances. Experts emphasize the importance of persistence, with health policy advocates urging patients to push through denials by leveraging every available resource. The complexity of insurance paperwork, often laden with jargon and buried instructions, further discourages action. In the D.C. area, however, local programs aim to bridge this gap by offering guidance and support. Understanding that external appeals are not just a formality but a legally backed process can empower patients to stand up against unjust decisions. This right, though underutilized, has proven to be a game-changer for those who navigate it successfully, highlighting the need for broader education on how to access and utilize this powerful tool.
2. Regional Resources for Navigating Appeals
In Maryland, patients facing insurance denials can turn to the Office of the Attorney General’s Health Education and Advocacy Unit, which provides free assistance with claims disputes, billing issues, and policy cancellations. A recently enacted law in the state mandates that insurers display appeal instructions prominently in bold type at the top of denial letters, ensuring clearer communication. This change mirrors efforts in other states like Connecticut, where similar reforms led to a 40% surge in filed appeals due to better-informed patients. This unit serves as a critical ally for residents, helping to demystify the often opaque appeal process and offering hands-on support to those who might otherwise abandon their claims. With such resources, Maryland stands out as a model for consumer protection in healthcare, ensuring that patients have a fighting chance against unfair coverage decisions.
Washington, D.C., also offers robust support through the Office of the Health Care Ombudsman and Bill of Rights, which assists residents with coverage denials and unresolved insurance disputes. Additional help is available via the Department of Health Care Finance for Medicaid concerns and DC Healthy Families for children’s coverage issues. These programs guide individuals through both internal and external appeal procedures, ensuring that no one is left to navigate the system alone. Meanwhile, Virginia, though no longer part of the federal Consumer Assistance Program, directs residents to the State Corporation Commission’s Bureau of Insurance for private plan complaints. Support for Medicaid, children’s health coverage through FAMIS, and Medicare is accessible via dedicated state programs like the Virginia Insurance Counseling and Assistance Program. These regional resources collectively form a safety net for D.C. area residents, providing tailored assistance to address the unique challenges of insurance denials across different jurisdictions.
3. Barriers to Accessing Appeal Rights
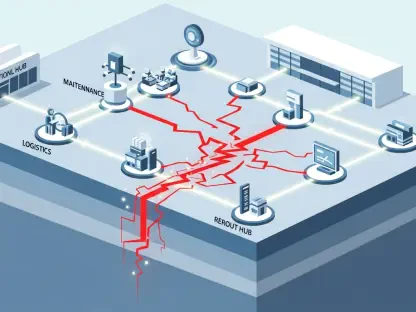
One of the most pressing challenges in the external appeal process is the low number of patients who pursue it, often due to sheer frustration and exhaustion, particularly among those battling severe illnesses like cancer. The emotional and physical toll of a health crisis can sap the energy needed to fight an insurance denial, leading many to abandon their claims prematurely. Compounding this issue is the lack of clarity in denial letters, which frequently fail to explain the appeal process in an accessible way or provide clear directions on next steps. Health advocates note that this opacity is a significant deterrent, as patients are left confused and discouraged by bureaucratic hurdles. The result is a system where only a fraction of those eligible for external reviews actually pursue them, allowing insurers to avoid accountability in numerous cases.
Beyond individual challenges, systemic issues exacerbate the problem, as insurers increasingly use denials as a cost-control tactic, banking on patients’ lack of follow-through. Health policy experts argue that without widespread awareness and stronger enforcement, this trend will persist, leaving vulnerable populations at risk of losing access to critical care. The complexity of the healthcare system itself adds another layer of difficulty, with many lacking the expertise to navigate appeals without assistance. In response, consumer assistance programs in the D.C. area strive to fill this gap, but their reach remains limited by funding and public knowledge of their existence. Addressing these barriers requires not only better communication from insurers but also a concerted effort to educate patients about their rights and the resources available to support them in their fight for coverage.
4. Practical Steps to Challenge a Denial
When faced with a coverage denial, taking immediate and strategic action is crucial to increasing the chances of a successful outcome. Experts recommend the following steps to navigate the process effectively: First, retain all documents related to the claim, as these records are essential for building a case. Second, request complete copies of claim files from the insurer to understand the specific reasons behind the denial. Third, seek free support by contacting a consumer assistance office, which can provide guidance and resources at no cost. Finally, challenge every denial by filing an appeal, as many issues stem from simple errors like coding mistakes that can be rectified with persistence. These steps, while straightforward, require diligence and attention to detail, but they can make a significant difference in overturning an unfair decision.
For cases involving urgent or complex medical needs, federal regulations permit expedited reviews, which must be resolved within 72 hours, ensuring swift action when time is of the essence. If the independent reviewer rules in the patient’s favor, insurers are legally obligated to cover the treatment, providing a critical safeguard for those in dire circumstances. Patients should also be aware that many disputes arise from clerical errors, which can often be resolved quickly once identified through the appeal process. Assistance from state programs in the D.C. area can be instrumental in drafting appeals and navigating these timelines. By following these actionable steps and leveraging available support, individuals can transform a denial from a dead end into an opportunity for resolution, ensuring that their right to necessary care is upheld against insurer resistance.
5. Advocacy and Support as Key Allies
Health advocacy organizations play an indispensable role in helping patients overcome the daunting task of challenging insurance denials, often stepping in to provide hands-on assistance. Groups like the Community Service Society have been known to draft detailed appeals on behalf of patients, sometimes sifting through thousands of pages of medical records to construct compelling cases spanning 15 to 20 pages. This level of support can be a game-changer for individuals who lack the time, energy, or expertise to navigate the system alone. By offering tailored guidance and leveraging their knowledge of healthcare policies, these organizations empower patients to stand up to insurers and secure the coverage they deserve. Their work highlights the importance of having expert allies in a landscape where denials are increasingly used as a financial strategy by insurance providers.
Beyond individual case support, broader advocacy efforts focus on raising public awareness and pushing for stricter enforcement of appeal rights to counter systemic inequities in healthcare access. Health policy leaders stress that every state should have robust consumer assistance programs to guide residents through the complexities of insurance disputes. Without such initiatives, many are left vulnerable to the intricacies of a system that can feel impenetrable. In the D.C. area, existing programs serve as a foundation, but their impact could be amplified through increased funding and outreach. The combined efforts of advocacy groups and state resources underscore a critical truth: patients are not alone in their fight for care, and with the right support, they can navigate even the most challenging denials to achieve a just outcome.
6. Moving Forward with Empowerment
Looking back, the struggle against insurance denials in the D.C. area revealed a landscape where external appeals stood as a beacon of hope for many, yet remained out of reach for others due to persistent barriers. Patients who tapped into this process often found relief, securing coverage for treatments that were initially rejected by insurers. State programs in Washington, D.C., Maryland, and Virginia played a pivotal role, offering guidance that turned despair into determination for countless individuals. The success stories of those who persevered through the appeal process served as a reminder of what was possible when resources and resolve aligned. Moving forward, the focus must shift to expanding access to information and support, ensuring that every resident knows their rights and how to exercise them. Strengthening consumer assistance programs and advocating for clearer insurer communication are essential next steps to dismantle the obstacles that once stood in the way of fair treatment access.