In recent years, the debate surrounding the use of artificial intelligence (AI) in health insurance claim denials has gained considerable traction, given its profound implications. With individuals like Remi Lee spotlighting the struggle against frequent claim denials, the conversation has gained urgency. Lee, born with caudal regression syndrome, a condition affecting lower body development, frequently faces rejections for essential medical needs, which her health insurance company often mislabels as mere “luxuries.” Her experiences have drawn attention to the potential role AI plays in accelerating denials, thereby emphasizing concerns over the effectiveness and fairness of these automated systems. As more claim denials are overturned upon appeal, questions arise regarding the legitimacy of initial rejections and the underlying processes fueling such decisions within the industry.
Controversy Surrounding Insurers and AI Use
Insurer Denials of AI Implementation
Despite growing suspicions and substantiated allegations, many insurers deny the use of AI systems for processing medical claim denials, maintaining that they employ human oversight. Nonetheless, ongoing class-action lawsuits suggest that major health providers are implementing AI in place of licensed physicians, fueling public skepticism about the feasibility of AI accurately processing claims in minimal time. The skepticism is further amplified by the rapid growth and complexity of insurance claims that require nuanced decision-making beyond the capabilities of present AI technologies. However, proving whether AI makes primary decisions or merely assists human professionals remains a challenging endeavor, requiring deeper examination by legal entities and regulatory authorities.
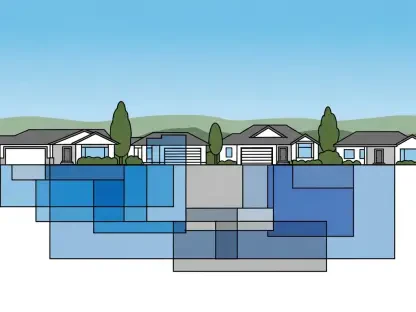
Regulatory Scrutiny and Industry Response
The increasing incorporation of AI into sectors like Medicare Advantage plans has prompted federal and state agencies to heighten scrutiny around AI’s application. Regulators are reviewing the scope and effectiveness of AI algorithms in claim processing to ensure they uphold ethical standards and deliver fair outcomes. As a result, insurance companies are under pressure to enhance transparency and accountability in their operations, demonstrating how algorithms affect claim decisions. This scrutiny fosters a need for balancing technological advancements with regulatory oversight to create a fair playing field for all stakeholders involved. Nonetheless, the challenge lies in crafting fair regulations that do not stifle innovation while protecting the rights of those dependent on insurance for critical medical needs.
Empowering Patients Through AI Innovations
Technological Solutions for Contesting Denials
Responding to the controversial use of AI by insurers, individuals like Holden Karau are harnessing AI technology to fight back against perceived unjust claims denials. Karau developed AI-driven tools that help patients generate targeted appeals, allowing them to craft well-informed counterarguments against insurance rejections. These innovations are proving significant for patients who often lack the resources or know-how to effectively contest denials through conventional channels. Such tools are emblematic of a broader trend where AI empowers consumers, providing them new avenues to challenge decisions once considered binding, thus democratizing the resolution process by granting individuals greater control over their healthcare situations.
Potential for Greater Patient Advocacy
The emergence of AI-driven strategies advocates for a technological equilibrium, where AI not only serves insurers but also aids policyholders in advocating for themselves. By developing solutions that enable patients to navigate the often-convoluted claims system, AI has the potential to reshape healthcare advocacy from a predominantly reactive stance to one that is proactive and informed. This shift equips patients with the necessary tools and insights to better understand their insurance policies, ultimately reducing the disparity between those who can and cannot effectively address denied claims. Patient advocacy in the face of digital transformation is increasingly crucial in ensuring that technology serves to enhance, rather than hinder, equitable access to necessary medical resources.
The Road Ahead in Healthcare AI
Despite increasing doubts and backed-up claims, many insurance companies refute the use of AI systems for handling medical claim denials, asserting that they rely on human oversight. Still, ongoing class-action lawsuits cast doubt, suggesting that significant health providers might be replacing licensed doctors with AI technology. This practice heightens public skepticism about AI’s capability to swiftly process claims. As claims grow in volume and complexity, effective decision-making demands a level of sophistication that current AI technologies struggle with. The challenge persists in determining whether AI is making primary decisions or merely assisting human professionals, a task that legal bodies and regulatory agencies need to scrutinize further. Unraveling the extent of AI’s role involves navigating complex technological and legal challenges, underscoring the need for transparency rules and rigorous analysis. The lingering question is: how deeply does AI intertwine with crucial healthcare decision-making?