We’re joined today by Simon Glairy, a leading expert in risk management and insurance law, to dissect a recent Delaware Supreme Court decision with significant implications for workers’ compensation. The case of a Wilmington firefighter, Corey Ferrell, brings into sharp focus the complex interplay between prior injuries, settlement agreements, and new workplace incidents. We’ll explore the critical evidence that distinguishes a new injury from a simple recurrence, the specific legal standards courts use to assign liability, and the powerful, file-closing finality of a well-drafted commutation agreement. This conversation will unpack the practical steps adjusters take when investigating these claims and what this ruling means for insurers and employees alike.
The Industrial Accident Board credited Dr. Matz’s opinion that the 2023 incident was a recurrence. Can you walk me through the key evidence, like the MRI findings or the nature of the stair-climb, that typically helps a court differentiate a compensable new injury from a non-compensable recurrence?
Absolutely, and this case is a masterclass in how that distinction is made. It really comes down to a battle between objective medical evidence and the subjective nature of the incident itself. The MRI evidence was paramount here. When the December 2023 MRI showed disc protrusion and herniations in the very same thoracic region implicated back in 2015, that’s a powerful piece of objective data for the defense. It allows an expert like Dr. Matz to paint a compelling picture of a degenerative progression, essentially arguing that the underlying condition was always there and just became more symptomatic. If the new MRI had shown a completely different injury at a new vertebral level, the case for a “new injury” would have been infinitely stronger. Then you look at the incident—carrying high-rise packs up three flights of stairs. For a firefighter, that’s not an accident; it’s a Tuesday. The Board saw this not as a distinct, “untoward event” but as an ordinary duty, which makes it much harder to argue it caused a new pathological change. The combination of matching medical imaging and a routine work activity created a very high hurdle for the claimant to clear.
The Supreme Court applied the Nally test for carrier liability over the Duvall test for pre-existing conditions. Could you break down the practical difference between these standards and share a hypothetical example of a case where applying the Duvall test would have led to a different outcome?
This is a subtle but crucial legal point that often determines who pays. Think of it this way: the Nally test is for when you already have a recognized, work-related injury, and you’re trying to decide if new symptoms belong to that old claim or a new one. It’s an allocation dispute between insurance carriers, or in this case, between an old carrier and a new employer. The Duvall test, on the other hand, is used to decide if a non-work-related, pre-existing condition becomes a compensable workers’ compensation claim for the first time because of normal job duties. The court correctly saw Ferrell’s situation as a Nally problem because his original 2015 injury was already a compensable work claim.
Now, for a hypothetical where Duvall would change things: Imagine if Ferrell’s 2015 back injury wasn’t from a work-related crash but from a personal car accident on his day off. He has this known, non-industrial back condition. Then, in 2023, he performs his ordinary duty of carrying the packs and his back flares up. In that scenario, the Duvall test would be the star of the show. The court would have to decide if the usual exertion of his job was enough to light up that pre-existing, non-work condition to the point that it now becomes a compensable injury against his current employer, the Wilmington Fire Department. The outcome could very well have been a new claim awarded against Wilmington, because the core question would shift from “which carrier is responsible?” to “is this incident compensable at all?”
Ferrell’s 2018 commutation was central to the final decision. What are the step-by-step best practices for drafting a commutation agreement to ensure it truly closes future liability? Conversely, what specific language should a claimant’s attorney scrutinize to protect their client from future coverage gaps?
The power of that 2018 commutation really can’t be overstated; it was the final nail in the coffin for this claim. For an insurer, the best practice is to use expansive and unequivocal language. You want phrases like “global commutation” and a specific release from “any and all future benefit liability” arising from or related to the original injury. You should explicitly list the body parts involved—in this case, the thoracic and cervical spine. A truly ironclad agreement will also state that it covers not just recurrences, but also aggravations, exacerbations, and any sequelae of the 2015 injury. The goal is to leave no ambiguity, making it clear that the claimant is accepting a sum of money in exchange for closing that chapter forever.
From the claimant’s attorney’s perspective, the job is to do the opposite: scrutinize every word for a potential loophole. You have to push back against overly broad language. For instance, an attorney might argue to limit the release to “natural recurrences” of the exact 2015 pathology, while attempting to preserve the right to file a claim for a “new and distinct traumatic injury” to the same body part. You’d also want to ensure the agreement doesn’t waive rights to unrelated medical conditions that could develop later. It’s a delicate dance. The claimant gets a lump sum payout and certainty, but they need to understand they are potentially walking away from a future safety net for that body part, so the language must be as narrowly tailored as possible to protect them from unforeseen circumstances.
The court found carrying high-rise packs was an ordinary duty, not a distinct “untoward event,” despite Ferrell reporting a “pop” in his back. What specific factors do adjusters and boards weigh when deciding if an incident is a new injury versus the manifestation of a pre-existing condition under normal exertion?
Adjusters and boards are trained to look past the subjective sensation, like a “pop,” and analyze the mechanics of the event. A “pop” can be felt during a degenerative flare-up just as easily as during a new traumatic event. The first factor they weigh is foreseeability. Is carrying heavy equipment up stairs a normal, expected part of a firefighter’s job? Yes. This immediately pushes it away from the “untoward event” category. An untoward event has to be something unusual or unexpected—a slip on an oil slick, a collapsing scaffold, a piece of equipment malfunctioning. The second factor is the presence of an external force. Here, the force was generated by Ferrell himself as part of his duties. There was no outside, intervening agent that acted upon him. Finally, they look at the consistency of the reporting. The article notes the timeline of Ferrell’s report of the “pop” was unclear in the records. That kind of ambiguity weakens its evidentiary value significantly. An adjuster hears “pop” and immediately thinks, “Okay, but what caused the pop?” If the cause was just doing the job you do every day, it points overwhelmingly toward a manifestation of the underlying, pre-existing condition.
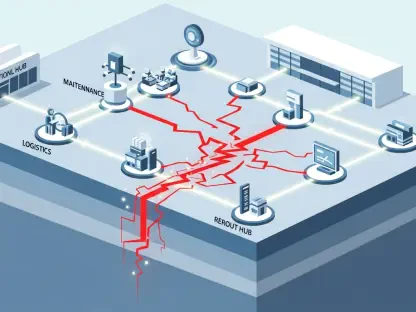
This ruling seems to be a significant win for insurers. When a worker with a prior commuted claim reports a new incident involving the same body part, what is the typical investigative process an adjuster follows, and what specific red flags immediately point toward a potential denial?
This is indeed a major win, and it reinforces a very clear investigative path for adjusters. The moment a claim comes in and the system flags that the claimant has a prior injury to the same body part, a series of red flags go up. The very first step is to pull the entire file for that old claim. The biggest red flag of all is finding a commutation agreement, especially a global one like Ferrell’s from 2018. That document immediately becomes the foundation of the defense. The next step is a detailed, recorded statement with the claimant, focusing intently on the mechanism of injury. We’re listening for words that signal an accident versus exertion. Did you slip? Did you trip? Did something fall on you? The absence of a clear, external, and unexpected event is the second major red flag. Simultaneously, we are ordering all the medical records, old and new. When we get that new MRI report and lay it side-by-side with the one from 2015 and see the damage is in the exact same thoracic region, that’s the third, and often final, red flag. At that point, the story is clear: a commuted claim, an incident involving normal work duties, and overlapping medical evidence. The path to denial becomes very well-defined.
What is your forecast for how rulings like this will shape future commutation negotiations between carriers and claimants?
My forecast is that rulings like Ferrell will add a significant amount of leverage for carriers at the negotiating table, but it will also force a higher level of sophistication from both sides. For insurers, this case becomes a powerful exhibit—Exhibit A, really—to demonstrate the true finality of a commutation. They can point to this decision and argue for a lower settlement amount, justifying it by saying, “We are taking on the full and final risk here, and the court has affirmed that ‘final’ means final.” Conversely, I predict claimant attorneys will become even more meticulous. They will likely demand higher settlement figures to compensate their clients for the very real risk of being left without coverage for a future flare-up, as happened to Ferrell. We may also see more attempts to write specific “carve-out” language into agreements, explicitly preserving the right to file for a new, distinct traumatic injury. Ultimately, it will make both sides sharpen their pencils, leading to tougher, more detailed negotiations where the long-term risks are priced into the settlement with much greater precision.