Medicare, a federal health insurance program primarily serving individuals aged 65 and older as well as certain younger people with disabilities, could potentially save $7.7 billion by aligning payments to Critical Access Hospitals (CAHs) for swing-bed services with the fee-for-service (FFS) prospective payment system rates. This discovery, brought to light by a recent audit conducted by the Office of Inspector General (OIG), has ignited a crucial debate about balancing cost-efficiency and ensuring access to healthcare in rural areas. The findings indicate that reevaluating the reimbursement structure for CAHs could offer substantial financial relief for Medicare, but the complexities of rural healthcare access must not be overlooked.
The Role of Critical Access Hospitals
Critical Access Hospitals (CAHs) play a vital role in providing essential healthcare services to rural communities, where access to medical care is often limited. Established under the Balanced Budget Act of 1997’s Rural Flexibility Program, CAHs are reimbursed by Medicare at 101% of their reasonable costs for hospital and swing-bed services. Swing-bed services, which enable hospitals to use beds interchangeably for acute and skilled nursing care, offer flexibility in patient care and help meet the diverse healthcare needs of rural populations.
The rationale for the higher reimbursement rates for CAHs is to ensure their financial viability, enabling them to continue serving their communities effectively. The primary goal is to make sure that rural residents do not face a lack of medical care due to the financial instability of local healthcare facilities. However, the recent OIG audit has raised concerns about the necessity of these higher rates, especially when there are other facilities offering similar services within a reasonable distance.
Findings of the OIG Audit
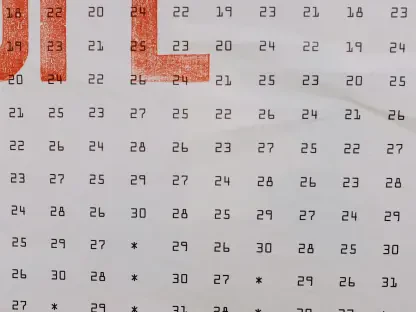
The OIG audit scrutinized the use of swing-bed services for skilled nursing care at CAHs from 2015 to 2020. During this period, an increase of 2.8% was observed in swing-bed usage, accompanied by a remarkable 16.6% rise in the average daily reimbursement for these services. The audit also reviewed a sample of 100 CAHs and found that 87 of these hospitals were located within 35 miles of alternative facilities providing equivalent skilled nursing services.
These findings suggest that many CAHs might not be the sole option for patients requiring skilled nursing care. If Medicare payments to CAHs for swing-bed services were aligned with FFS prospective payment system rates, considerable savings could be realized without compromising patient access to necessary care. This potential for savings has set off discussions about whether the continued financial support for CAHs, at their current reimbursement rates, is justifiable when alternatives exist.
Potential Savings and Legislative Changes
The OIG has recommended that the Centers for Medicare & Medicaid Services (CMS) pursue legislative changes to bring CAH reimbursement rates in line with those of alternative facilities offering similar services. This realignment could potentially save billions for Medicare, funds which could be redirected to other pressing needs within the healthcare system, thus enhancing overall healthcare delivery.
However, the CMS has expressed reservations regarding the OIG’s proposals, citing concerns about the audit’s methodology and the potential adverse impact on rural communities. From their perspective, reducing reimbursement rates for CAHs could jeopardize the financial sustainability of these hospitals, leading to closures and diminished access to healthcare services for rural residents. This poses a significant challenge, as these hospitals are often the lone providers of medical care in their respective areas.
Balancing Cost-Efficiency and Rural Healthcare Access
The dialogue surrounding the alignment of CAH swing-bed payment rates with FFS rates underscores a larger dilemma: the balance between achieving cost-efficiency and ensuring sustained access to healthcare in rural regions. On one hand, the potential savings for Medicare are substantial and could contribute to the long-term financial health of the program. On the other hand, slashing payments to CAHs risks undermining the primary purpose of these institutions, which is to deliver critical healthcare services to populations that are already underserved.
Policymakers must weigh the potential consequences of implementing changes to CAH reimbursement rates very carefully. While there is a clear imperative to realize cost savings, this goal must be measured against the potential impact on rural healthcare access. Ensuring that rural residents continue to receive essential medical care should remain a key consideration in any proposed adjustments to the reimbursement model.
The Future of CAH Reimbursement Rates
As the discussion progresses, it becomes evident that any modifications to CAH reimbursement rates will require thorough planning and consideration. Engaging diverse stakeholders, including rural healthcare providers, patients, advocacy groups, and policymakers, will be crucial in crafting changes that preserve access to care while tapping into potential cost savings.
One potential strategy could involve a gradual reduction in reimbursement rates, which would provide CAHs with the necessary time to adapt and explore alternative revenue sources. Additionally, providing targeted support and incentives to CAHs that demonstrate a commitment to maintaining high-quality care and improving efficiency could help mitigate any negative impacts.
Conclusion
Medicare, the federal health insurance program primarily catering to individuals aged 65 and older, as well as certain younger people with disabilities, could save a substantial $7.7 billion by adjusting how it pays Critical Access Hospitals (CAHs) for swing-bed services. By aligning these payments with the fee-for-service (FFS) prospective payment system rates, considerable savings could be achieved. This new finding, revealed by a recent audit from the Office of Inspector General (OIG), has sparked an essential debate about finding the balance between cost-efficiency and maintaining healthcare access in rural areas. Analysts suggest reevaluating the reimbursement structure for CAHs, but stress that policymakers must carefully consider the intricate nature of healthcare access in these communities. Redefining the payment system could bring significant financial relief to Medicare, but it is imperative that the unique healthcare needs of rural areas remain at the forefront of any decision.