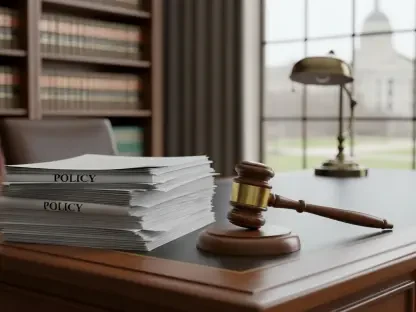
The solemn promise of an insurance policy is to provide a financial safety net in a time of crisis, a promise a West Virginia couple alleges was systematically broken not by human error, but by calculated technological design. A landmark lawsuit filed on January 7, 2026, accuses Liberty Mutual Insurance Company and several of its technology partners of engaging in a coordinated scheme to intentionally underpay policyholders. The case, brought by Edward and Tammy Lynn Ryan, has sent ripples through the insurance industry, questioning whether the push for technological efficiency has come at the expense of policyholder trust. The complaint, filed in the US District Court for the Northern District of West Virginia, names Liberty Mutual, CCC Intelligent Solutions Inc., Snapsheet Inc., and Claim Assist as defendants in a case that could reshape how claims are processed nationwide.
When Technology Fails the Policyholder
For the Ryans, the nightmare began after an April 2025 tornado tore through Morgantown, leaving extensive damage to their home and five vehicles. Relying on their insurance policy to begin the difficult process of rebuilding, they initiated a claim with Liberty Mutual. However, the response they received was not one of support, but of shock and disbelief. The insurer’s initial offer for the extensive home damage was a mere $24,304, a figure that stood in stark contrast to an independent public adjuster’s assessment, which valued the necessary repairs at $160,127.
This staggering disparity forms the crux of the lawsuit and raises a critical question for millions of policyholders: Is the technology marketed to streamline and simplify the insurance claim process—from virtual photo appraisals to AI-driven assessments—actually engineered to reduce the final payout? The Ryans’ legal battle contends that this is not an unfortunate bug in the system but a deliberate feature designed to benefit the insurer’s bottom line.
The Rise of Insurtech and Automated Appraisals
The insurance industry has undergone a significant transformation, rapidly shifting toward “Insurtech” solutions. Companies are increasingly integrating artificial intelligence, virtual appraisal platforms, and third-party software into their core operations. To consumers, this evolution is presented as a clear win, promising a faster, easier, and more efficient claims process that replaces cumbersome paperwork and lengthy waits with digital simplicity.
However, this technological pivot introduces a potential conflict of interest that lies at the heart of the Ryans’ allegations. The lawsuit claims that when insurers outsource critical claims functions to tech vendors whose business models are built on delivering “indemnity savings,” the vendor’s primary incentive is to minimize claim payments. This arrangement creates a dynamic where the technology partner is financially rewarded for outcomes that are directly detrimental to the policyholder it is supposed to be serving impartially.
Anatomy of an Alleged Underpayment Scheme
The core allegation detailed in the complaint is a coordinated effort between Liberty Mutual and its tech partners to systematically and fraudulently underpay claims. The lawsuit meticulously breaks down the role each company allegedly played in this process, painting a picture of a system designed to work against the policyholder from the moment a claim is filed.
At the center of the vehicle claims process was Snapsheet, whose virtual appraisal services are marketed to insurers with the promise of “15-20% Indemnity Savings.” The complaint alleges that Snapsheet trains its estimators to intentionally conceal poor photo quality submitted by customers, leading to incomplete and inaccurate damage reports. For total loss valuations, the lawsuit scrutinizes CCC Intelligent Solutions, highlighting disclaimer language in its reports that labels its valuation as a mere “opinion.” The Ryans’ filing argues this language is used to abdicate responsibility and prove the assessments were not independent. The complaint also targets Claim Assist, whose AI-powered platform allegedly uses a scoring system to financially incentivize a network of adjusters and contractors to close claims as quickly and cheaply as possible.
By the Numbers: A Stark Financial Reality
The financial figures outlined in the legal filing reveal the severe impact of these alleged practices on the Ryan family. The nearly $136,000 gap between Liberty Mutual’s initial estimate and the public adjuster’s findings for the home damage represents the most significant discrepancy. This difference alone highlights a fundamental breakdown in the valuation process.
The underpayments extended beyond the structural damage. According to the complaint, a personal property claim exceeding $11,000 was never properly reviewed by the insurer. The auto claims were similarly affected, with the most glaring example being the payment for a 2019 Cadillac Escalade, which amounted to just $212.67 after the deductible was applied. In response to these outcomes, the Ryans are seeking compensatory and punitive damages through claims of bad faith, civil conspiracy, fraud, and breach of contract.
What Every Policyholder Should Know Before Filing a Claim
This case serves as a critical reminder for consumers to approach the claims process with diligence and a healthy dose of skepticism. It is essential to understand that an initial offer from an insurer, especially one generated through a virtual or automated process, may not be complete or final. Policyholders should not feel pressured to accept the first figure presented.
Maintaining meticulous records is paramount. Document every communication with the insurer and its vendors, save all photos and reports, and take detailed notes during conversations. If the damage is significant or the initial offer seems unreasonably low, it may be necessary to hire an independent public adjuster. These professionals work for the policyholder, not the insurance company, and can provide an unbiased assessment of damages. Finally, it is crucial to review your policy and any third-party reports used to evaluate your claim, paying close attention to the fine print and disclaimer language that could impact your final payout.
This lawsuit is a stark illustration of the potential pitfalls in an increasingly automated industry. The outcome of the case and its influence on regulatory oversight could determine whether technology becomes a tool for greater transparency or an instrument for systemic underpayment, fundamentally altering the relationship between insurers and the policyholders who depend on them. The proceedings have revealed a need for consumers to remain vigilant and advocate for their rights in a landscape where algorithms and automated systems play a growing role in determining financial futures.