Setting the Stage for Market Analysis
In an era where financial security for disabled individuals hangs in a delicate balance, a high-profile legal battle has emerged as a focal point for the disability insurance market, highlighting systemic issues. A significant lawsuit filed by a former school district employee against major players like Tokio Marine Holdings, Inc., Reliance Standard Life Insurance Company, and Matrix, alongside other administrators, has spotlighted critical flaws in claims handling. This case, lodged in a federal court, alleges wrongful denial of benefits under the Employee Retirement Income Security Act (ERISA), accusing insurers of arbitrary denials, fraud, and systemic misconduct. Such allegations are not isolated but reflect broader concerns within an industry managing billions in premiums annually. This analysis aims to dissect current trends in disability claims denials, explore data-driven insights, and forecast potential shifts in market practices and regulations, shedding light on what stakeholders can expect in this evolving landscape.
Deep Dive into Disability Insurance Market Dynamics
Current Trends in Claims Denials and Legal Challenges
The disability insurance sector, valued at over $30 billion in annual premiums in the United States, is grappling with a surge in legal challenges over claims denials. Recent data indicates that nearly 30% of long-term disability claims are denied on initial submission, with a significant portion of these denials contested in court for alleged unfair practices. High-profile lawsuits, such as the one involving a former employee of Rockford School District 205, underscore a growing frustration among claimants who argue that insurers prioritize cost-cutting over fiduciary duty. These legal battles often cite inconsistent medical evaluations and lack of transparency as core issues, painting a troubling picture of trust erosion between policyholders and providers. As litigation costs mount, insurers face not only financial risks but also reputational damage in a market increasingly sensitive to consumer advocacy.
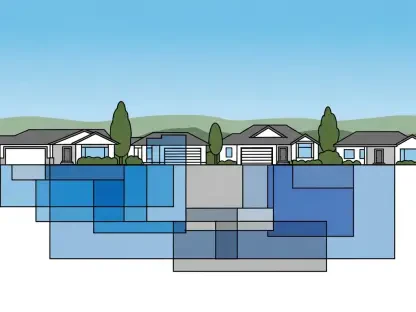
Data Insights: Denial Rates and Industry Practices
Analyzing industry data reveals stark disparities in denial rates across insurers and regions, with some companies reporting denial percentages as high as 40% for certain disability plans. Reports from regulatory bodies suggest that internal medical reviews, often conducted by company-selected physicians, contribute heavily to these figures, raising questions about impartiality. For instance, discrepancies between independent medical opinions and insurer assessments have fueled accusations of systemic bias, a concern echoed in numerous ERISA-based lawsuits. Furthermore, smaller insurers tend to exhibit higher denial rates compared to larger conglomerates, possibly due to limited resources for thorough claims processing. This data highlights a critical need for standardized evaluation protocols to ensure fairness, as inconsistent practices could drive policyholders toward alternative financial safety nets or legal recourse.
Projections: Regulatory Reforms and Market Shifts
Looking ahead, the disability insurance market is poised for transformative changes driven by mounting legal pressures and advocacy for stricter oversight. Projections suggest that between 2025 and 2027, federal regulators may introduce enhanced ERISA compliance guidelines, potentially mandating independent third-party medical reviews to curb biased denials. Insurers might also adopt technology, such as AI-driven claims analysis, to streamline processes and reduce human error or subjectivity, with adoption rates expected to rise by 15% over the next few years. Additionally, the growing wave of lawsuits could push premium costs upward as companies offset litigation expenses, a trend that may disproportionately affect small businesses offering group plans. These shifts signal a market at a crossroads, balancing profitability with the imperative for equitable treatment of claimants.
Reflecting on Market Insights and Strategic Pathways
Reflecting on the comprehensive analysis conducted, the disability insurance market faces significant scrutiny over claims denials, with legal battles exposing potential systemic flaws in handling processes. The data underscores a troubling trend of high denial rates and inconsistent medical evaluations, while projections point to a future shaped by regulatory reforms and technological integration. These findings illuminate the urgent need for insurers to reassess their claims management strategies to rebuild trust with policyholders. Moving forward, stakeholders are encouraged to prioritize transparency by adopting independent review mechanisms and leveraging digital tools for objective decision-making. Additionally, collaboration with regulatory bodies to establish uniform standards could mitigate risks of litigation and enhance market stability. This strategic focus on fairness and innovation offers a pathway toward a more resilient disability insurance sector, ensuring protection for those who need it most.