Imagine a couple sitting at their kitchen table, poring over medical bills and insurance policies, desperately trying to figure out how to afford in vitro fertilization (IVF) that costs upward of $15,000 per cycle, knowing that their dream of starting a family hangs in the balance. This scenario plays out for countless Americans grappling with infertility, a condition affecting one in six adults worldwide, as reported by the World Health Organization. The financial strain of fertility treatments can be overwhelming, and the pressing question remains whether health insurance offers any relief. In the U.S., the answer isn’t a simple yes or no—it’s a tangled web of state laws, federal guidelines, employer decisions, and plan specifics that create a frustratingly uneven landscape. For many, understanding coverage feels like navigating a maze blindfolded, with hope often hinging on where they live or what kind of insurance they have. This article aims to untangle that complexity, exploring the nuances of coverage for IVF and other fertility treatments, from federal shortcomings to state-by-state differences, and offering practical insights for those seeking answers. Let’s dive into the heart of this issue and shed light on what shapes access to these life-changing treatments.
Unpacking the Basics of Fertility Coverage
The Weight of Infertility and Its Costs
Infertility isn’t just a medical diagnosis; it’s a deeply personal struggle that carries a hefty price tag, often catching couples off guard when they realize the extent of out-of-pocket expenses. For many, treatments like IVF represent a beacon of hope, but a single cycle can cost between $15,000 and $20,000, with additional expenses for medications, diagnostic tests, and multiple attempts often pushing the total much higher. Without insurance support, these costs can derail dreams of parenthood, forcing tough choices between financial stability and family-building. The emotional toll compounds the challenge, as individuals wrestle with stress and uncertainty while trying to decipher if their health plan offers any lifeline. This reality underscores why understanding insurance benefits isn’t just a bureaucratic exercise—it’s a critical step in accessing care that can change lives.
Beyond the immediate sticker shock, the broader impact of infertility reveals why coverage matters so much. It’s not uncommon for couples to need several cycles of treatment, each with no guaranteed success, meaning expenses can balloon into the tens or even hundreds of thousands of dollars over time. Moreover, the lack of universal standards for what insurance must cover leaves many feeling isolated, as they watch peers in different states or with different plans receive benefits they can’t access. This disparity fuels a sense of inequity, amplifying the urgency to push for better policies and transparency. As the demand for fertility care grows, the conversation around affordability becomes impossible to ignore, setting the stage for a deeper look at how coverage varies across the nation.
The Patchwork of Coverage Across America
Navigating the landscape of fertility treatment coverage in the U.S. feels like piecing together a puzzle with missing parts, as policies differ dramatically depending on geography and plan type. Some states mandate insurance companies to cover certain aspects of infertility care, while others leave it entirely optional, creating a stark divide in access. On top of that, the kind of insurance—whether it’s an employer-sponsored plan, a Marketplace policy under the Affordable Care Act (ACA), or Medicaid—plays a massive role in determining benefits. This fragmentation means that two people with similar needs might face wildly different outcomes based solely on where they live or who they work for. It’s a system that often feels arbitrary, leaving many to wonder why something as fundamental as family-building support isn’t standardized.
Adding to the confusion, even within states that offer mandates, exceptions and fine print can limit who qualifies for coverage. For instance, self-insured employer plans, which cover a significant portion of workers, often fall outside state regulations, meaning employees in those plans might miss out regardless of local laws. Meanwhile, federal oversight provides no unifying mandate, leaving gaps that states and insurers fill—or don’t fill—at their discretion. This inconsistency isn’t just frustrating; it can be heartbreaking for those already navigating the emotional rollercoaster of infertility. As we peel back the layers of this complex system, it becomes clear that understanding these variations is the first step toward advocating for change and securing the support needed.
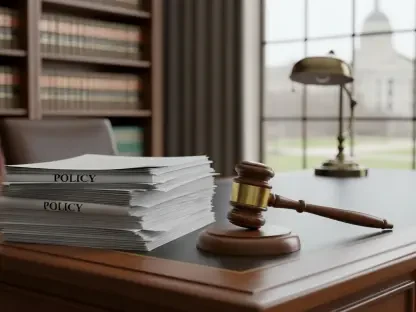
The Federal Role and Its Shortcomings
Absence of a National Standard
At the heart of the coverage conundrum lies a glaring federal gap: there’s no national requirement for health insurance plans to include IVF or other fertility treatments as a mandatory benefit. While the Affordable Care Act established a framework of 10 essential health benefits for individual and small-group plans, assisted reproductive technologies didn’t make the cut. This omission means that unless a state explicitly includes such care in its Essential Health Benefits (EHB) benchmark plan, insurers aren’t obligated to offer it. For millions of Americans, this federal silence translates to a lack of guaranteed support, pushing the burden onto states and private insurers to decide who gets help and who doesn’t. It’s a striking oversight in a healthcare system that often claims to prioritize comprehensive care.
This absence of a federal mandate creates a ripple effect, amplifying disparities across the country. Without a unified standard, individuals in states with weaker or nonexistent policies find themselves at a distinct disadvantage, often forced to pay out of pocket or forego treatment altogether. Even as advocacy groups push for legislative change, progress at the national level remains slow, with proposed bills to mandate coverage historically stalling in Congress. Meanwhile, the emotional and financial weight of infertility doesn’t pause for policy debates, leaving many to grapple with a system that feels indifferent to their needs. This federal inaction sets the tone for a broader discussion on how much—or how little—support is available, depending on where the responsibility falls next.
Current Federal Efforts and Their Limits
Though a national mandate remains elusive, recent federal initiatives have aimed to address the affordability of fertility treatments, albeit with significant constraints. Efforts under the Trump administration this year have focused on reducing prices for certain IVF medications and encouraging employers to offer optional stand-alone fertility benefits. These steps signal a recognition of the growing demand for support, yet they fall short of creating enforceable coverage requirements. Unlike comprehensive group health plans, these optional benefits often lack the consumer protections that ensure fair access and cost controls, leaving room for gaps in care. It’s a half-measure that highlights the ongoing challenge of balancing affordability with systemic change.
Moreover, the lack of binding federal policy means these initiatives rely heavily on voluntary participation from employers and insurers, which can lead to inconsistent outcomes. For those already struggling to navigate insurance complexities, such measures may offer a glimmer of hope but often fail to provide the robust safety net needed for treatments as costly and unpredictable as IVF. Legislative proposals introduced this year to mandate infertility coverage face an uphill battle, echoing past efforts that fizzled out amid political gridlock. This uncertainty at the federal level keeps the spotlight on states and employers to fill the void, reinforcing the fragmented nature of support for fertility care. As these efforts unfold, the limitations remind us that piecemeal solutions can’t fully address the deeper inequities at play.
State-Level Efforts and Disparities
Mandates in Place Across States
Diving into the state-level landscape, it’s clear that some regions are stepping up where federal policy falls short, with 25 states and the District of Columbia currently requiring at least some level of fertility treatment coverage for state-regulated health plans. Places like Massachusetts stand out with comprehensive mandates that include IVF and other assisted reproductive technologies, often capping cost-sharing to match non-fertility care. On the other hand, states like Arkansas offer more limited IVF coverage, with stipulations such as a $15,000 lifetime maximum and exclusions for certain plan types like HMOs. These variations reflect a broader reality: even where mandates exist, the depth and scope of benefits can differ drastically, shaping who gets help and how much.
Beyond these examples, the diversity in state approaches reveals a complex tapestry of intent and implementation. Some states focus on covering just the diagnosis of infertility, while others extend benefits to treatments or fertility preservation for medical conditions like cancer. This inconsistency can be a lifeline for residents in progressive states but a barrier for those elsewhere, where no such laws apply. For individuals moving between states or comparing options, these differences underscore the importance of knowing local regulations. As advocacy pushes for broader mandates, the current state-by-state picture offers both hope and frustration, illustrating how geography can dictate access to life-altering care in ways that feel profoundly unfair.
Restrictions and Gaps in State Policies
Even in states with coverage mandates, the fine print often reveals significant hurdles that can limit access for many seeking fertility care. A major stumbling block is the exemption of self-insured employer plans—covering about 67% of workers with employer-sponsored insurance—from state regulations. This means that even in areas with strong laws, a large swath of employees may find their plans unaffected by mandates, leaving them without benefits. Additionally, exceptions for religious employers or exclusions for treatments like reversing voluntary sterilization further narrow the pool of who qualifies. These restrictions paint a picture of partial progress, where well-intentioned policies don’t always translate to universal support.
Compounding these challenges are specific eligibility criteria that can catch individuals off guard. Some states require cheaper treatments, such as intrauterine insemination, to be attempted and fail before approving IVF coverage, while others impose waiting periods or age limits that exclude certain groups. These rules, though often designed to control costs, can feel like arbitrary gatekeeping to those already navigating emotional and physical strain. The result is a system where even mandated coverage comes with strings attached, forcing many to dig deeper into their own resources or give up on treatment altogether. As states grapple with balancing budgets and healthcare needs, these limitations highlight the ongoing tension between expanding access and maintaining fiscal caution.
Legislative Momentum and Future Prospects
Despite the gaps, there’s undeniable momentum at the state level, with several regions actively working to broaden fertility coverage through new laws and updated Essential Health Benefits benchmarks. Over the past few years, states like Colorado, Delaware, and California have introduced or enhanced mandates, reflecting a growing acknowledgment of infertility as a critical health issue. Looking ahead, pending legislation in places like Hawaii, New Jersey, and Vermont aims to expand IVF benefits, ensure access regardless of marital status, and cover preservation for broader medical conditions. This trend suggests a slow but steady shift toward recognizing fertility care as a fundamental need, even as progress varies in speed and scope.
However, not every effort crosses the finish line, as fiscal concerns and political opposition often stall promising bills. In some states, comprehensive proposals have been vetoed over budget impacts, while others face delays in legislative cycles that leave advocates in limbo. Still, the Department of Health and Human Services’ recent rules easing updates to EHB benchmarks could spur more states to add fertility benefits in the coming years, such as California’s planned expansion by 2027. This evolving landscape offers a mixed bag of optimism and caution, as each legislative win chips away at disparities, yet the patchwork nature of coverage persists. For those watching these developments, the message is clear: change is happening, but it demands patience and persistent advocacy to close the remaining gaps.
Employer and Marketplace Insurance Dynamics
Shifts in Employer-Sponsored Benefits
For nearly half of Americans, employer-sponsored insurance is the primary source of health coverage, and there’s a noticeable uptick in companies offering fertility benefits, particularly among larger firms. Surveys show that the percentage of employers providing such support jumped from 30% in 2020 to 42% in 2024, driven by competitive job markets and employee demand. This shift is a welcome relief for many, as it often includes coverage for IVF or related treatments that would otherwise be unaffordable. Yet, the catch lies in the distinction between fully insured and self-insured plans—while the former must adhere to state mandates, the latter face no such obligation, leaving coverage decisions entirely up to the employer’s discretion.
This variability within employer plans creates a frustrating dichotomy, where employees at one company might access robust fertility benefits while those at another, even in the same state, get nothing. For self-insured plans, which dominate among larger employers, the absence of state oversight means benefits hinge on corporate priorities, not legal requirements. Smaller businesses, often categorized under small-group plans, might follow state EHB benchmarks, but their offerings can still pale compared to larger competitors. As more employers recognize the value of fertility support in attracting talent, the trend is promising, yet it’s far from a universal fix. The uneven adoption leaves significant pockets of workers navigating infertility without the safety net they desperately need.
Marketplace Plans and Benchmark Standards
Turning to individual and small-group Marketplace plans, coverage for fertility treatments often ties directly to state-defined Essential Health Benefits benchmarks, which set the minimum standards insurers must meet. In states like Connecticut, Delaware, and the District of Columbia, these benchmarks include IVF, ensuring a baseline of support for those enrolled in ACA-compliant plans. However, the level of coverage and associated out-of-pocket costs can still vary based on the specific plan’s design, such as deductibles or copays. For individuals without employer insurance, these Marketplace options can be a critical resource, yet they’re only as strong as the state’s commitment to including fertility care in its standards.
In contrast, many states’ EHB benchmarks stop short of comprehensive benefits, offering only diagnostic coverage or nothing at all, which leaves Marketplace enrollees in those areas to shoulder the full cost of treatments. This disparity mirrors the broader state-level inconsistencies, where geography once again dictates access. Additionally, the financial burden of premiums and cost-sharing can make even covered treatments a stretch for some, underscoring the need for more uniform and generous benchmarks. As states like Washington plan to expand their EHB standards in the coming years, there’s potential for wider access through the Marketplace. Still, until those changes take root across more regions, many will find that shopping for individual coverage offers limited relief in the face of infertility’s high costs.
Public Insurance and Persistent Inequities
Scarcity of Support in Medicaid
When it comes to public insurance, the outlook for fertility treatment coverage under Medicaid is disheartening, with most states offering little to no help for procedures like IVF or intrauterine insemination. Across the board, Medicaid programs prioritize basic healthcare over specialized reproductive care, leaving out even diagnostic support in many cases. Rare exceptions exist—states like New York and the District of Columbia cover limited cycles of fertility medications, while Illinois and Utah provide preservation options before certain medical treatments like cancer therapy. For low-income individuals reliant on Medicaid, this near-total absence of benefits creates a stark barrier, often shutting the door on family-building options that others might access through private plans.
This lack of coverage isn’t just a policy gap; it’s a profound inequity that hits hardest for those already facing economic hardship. The inability to afford private insurance or out-of-pocket costs means many must forgo treatment entirely, perpetuating cycles of disadvantage. While pending legislation in a handful of states like Vermont and New Jersey aims to expand Medicaid benefits for fertility services, such reforms are far from widespread or guaranteed. The scarcity of public support highlights a systemic oversight, where the most vulnerable are left behind in a healthcare framework that struggles to address specialized needs. As debates over public funding continue, the reality for many on Medicaid remains one of exclusion from care that could transform their lives.
Broader Disparities in Access to Care
Beyond Medicaid’s limitations, disparities in fertility treatment coverage ripple through various dimensions, often tied to geography, income, and plan type, creating a deeply uneven playing field. Individuals in states without mandates or robust EHB benchmarks face steeper challenges, as do those under self-insured employer plans exempt from local laws. Rural residents might also struggle with fewer in-network providers, adding logistical hurdles to already complex financial barriers. These layers of inequity mean that access to IVF or other treatments often depends less on medical need and more on arbitrary factors like ZIP code or workplace, a reality that feels fundamentally unjust to many.
Compounding these issues is the intersection of socioeconomic status and cultural barriers, where marginalized groups may face additional obstacles in navigating insurance systems or advocating for coverage. For instance, single parents or same-sex couples encounter eligibility restrictions in some state mandates, further limiting their options. The cumulative effect is a system that disproportionately burdens certain populations, amplifying stress during an already vulnerable time. As policymakers and advocates push for reforms, addressing these disparities requires more than just expanding benefits—it demands a holistic look at how access is shaped by broader social and structural factors. Until then, the uneven distribution of support remains a glaring flaw in the pursuit of equitable healthcare.
Practical Steps for Securing Coverage
Essential Questions for Insurers and HR
Navigating the murky waters of insurance coverage for fertility treatments starts with asking the right questions, a step that can make all the difference in uncovering hidden benefits or avoiding unexpected costs. Contacting the health plan provider or human resources department to clarify if infertility benefits are included is crucial, as is understanding how the plan defines infertility itself—some policies have strict criteria that might exclude certain diagnoses. Additionally, inquiring about specific treatments covered, such as diagnostic tests, medications, or IVF cycles, helps paint a clearer picture of available support. Don’t overlook limits like the number of cycles allowed or lifetime dollar caps, as these can significantly impact planning. Finally, checking for in-network provider restrictions ensures that care is sought from approved facilities to maximize benefits.
Digging deeper, it’s also worth asking about any pre-authorization requirements or mandatory steps, like trying less invasive treatments before qualifying for IVF, which can delay or complicate the process. Clarifying whether coverage extends to fertility preservation for medical reasons, such as before cancer treatment, adds another layer of preparation, especially for those facing urgent health decisions. These conversations aren’t just about gathering facts; they’re about empowerment, equipping individuals with the knowledge to push back against denials or seek alternative options. Given the variability across plans and states, this proactive approach transforms a daunting system into a more manageable one, even if it requires persistence to get straight answers from often opaque insurance bureaucracies.
Decoding the Fine Print of Policies
Beyond asking questions, diving into the specifics of an insurance policy’s documentation can reveal critical details that conversations alone might miss, safeguarding against nasty financial surprises. Every plan has unique quirks—some might define covered treatments narrowly, excluding donor eggs or sperm, while others impose waiting periods before benefits kick in. Reviewing the summary of benefits and coverage, often available online or through HR, helps pinpoint these nuances. Pay close attention to cost-sharing structures, like copays or coinsurance, which can add up quickly during multiple treatment cycles. Understanding appeal processes for denied claims is equally vital, as it offers a recourse if initial coverage requests are rejected.
Taking this a step further, comparing in-network versus out-of-network costs can influence where treatment is sought, as sticking with approved providers often slashes expenses. For employer plans, checking if fertility benefits are part of a separate rider or optional add-on can explain why coverage isn’t immediately apparent. This meticulous review isn’t just paperwork—it’s a strategic move to align expectations with reality, especially since fertility care often spans months or years of unpredictable outcomes. Armed with this detailed understanding, individuals can better budget, advocate for themselves, and avoid pitfalls that derail both finances and hope. In a system where clarity is often lacking, becoming a detective of one’s own policy is a powerful way to regain some control over an uncertain journey.
Reflecting on Progress and Paths Forward
Lessons from a Fragmented System
Looking back on the journey through the maze of health insurance coverage for IVF and fertility treatments, it became evident that the U.S. healthcare system tackled this issue with a fragmented approach that left much to be desired. State mandates, while groundbreaking in places like Massachusetts and Connecticut, fell short for many due to exemptions for self-insured plans and the glaring lack of federal oversight. Employer initiatives showed promise, with a rising number of companies stepping up to offer benefits, yet disparities persisted for those under less progressive plans or public programs like Medicaid. Each layer of this system revealed both incremental victories and stubborn barriers that shaped countless personal stories of struggle and resilience.
Building Toward Equitable Access
Moving forward, the focus must shift to actionable solutions that bridge these persistent gaps and create a more inclusive framework for fertility care. Advocates and policymakers should prioritize federal legislation to establish a baseline of coverage, ensuring that no one’s access hinges solely on state lines or employer whims. States, meanwhile, can continue to lead by expanding mandates to cover self-insured plans and broadening eligibility criteria to include diverse family structures. Employers have a role too, by voluntarily adopting comprehensive benefits as a standard rather than a perk. For individuals, staying informed and pushing for transparency from insurers remains key—knowledge is power in a system rife with complexity. As society increasingly recognizes infertility as a medical need, not a luxury, these combined efforts could transform a patchwork of policies into a safety net that truly supports every dream of parenthood.