Policymakers, insurers, and families keep returning to a deceptively simple question that shapes budgets, benefits, and business models across the region: do Latin American constitutions actually require residents to buy health insurance, or do they merely set rights and leave the hard rules to ordinary statutes? The answer carries real consequences for enrollment strategies, employer obligations, and the boundaries between public guarantees and supplementary coverage, because a constitutional command would lock policy choices at the highest legal level, while a statutory approach would permit reform through ordinary legislative bargaining, administrative design, and judicial oversight that corrects gaps case by case as systems evolve and fiscal pressures shift.
1. Regional Baseline And Core Claim
Across Latin America, the constitutional baseline consistently favors a rights-first architecture: most charters recognize health as a fundamental entitlement and assign core duties to the State, but stop short of ordering individuals to purchase insurance. This structure sets direction and legitimacy without prescribing a single model, allowing legislatures and ministries to determine how systems reach universalism. The core claim is thus twofold. First, constitutions act as a compass by enshrining a right to health or health protection. Second, compulsory insurance, when present, usually arises from social security statutes and health codes. The split matters because it preserves room to calibrate contributions, subsidies, and provider roles as demographic and fiscal realities evolve.
Brazil’s 1988 Constitution illustrates the pattern. It states that health is a universal right and a State duty, and it grounded that promise in the Unified Health System, SUS, while leaving program design to legislation and policy. Mexico’s Article 4 recognizes the right to health protection, with the General Health Law and social security laws handling the operational details. Ecuador likewise lists health and social security among the State’s central duties and explicitly contemplates universal social protection, directing the State to organize systems that guarantee access. In all three, the constitutional text sets broad obligations and guardrails but avoids a personal purchase mandate, leaving that kind of compulsion—if any—to ordinary legal instruments.
2. Statutory Mandates, System Design, And Courts
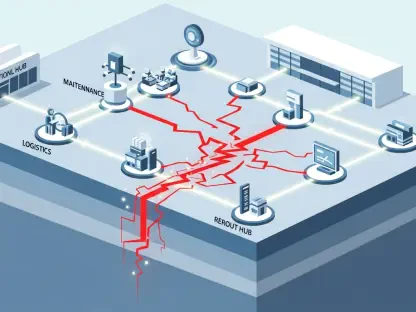
Where mandates exist, they are statutory rather than constitutional. Mexico enrolls formal-sector workers through social security legislation that specifies contributions, benefits, and administration. Colombia structures enrollment and benefit design through ordinary laws that regulate insurers and plans, defining who contributes, how subsidies are targeted, and what the benefit package contains. In practice, constitutions provide principles, while statutes and regulations translate those principles into enforceable rules about funding flows, risk pooling, and provider networks. That division lets governments adjust premium formulas, oversight tools, and contracting models without amending constitutional text, which is slower and politically costly.
This legal split also shapes enforcement. Courts have become pivotal in transforming rights on paper into real access. Colombia’s Constitutional Court, in Decision T-760 of 2008, declared health a fundamental right for all and ordered systemic fixes to align benefit catalogs, financing, and oversight with constitutional standards. The ruling pressed legislators and administrators to harmonize entitlements across regimes and strengthen supervision of payers and providers. Judicial review continues to function as a guardrail that closes coverage gaps, compels access to essential medicines, and curbs arbitrary denials, all while respecting the constitutional design that positions rights at the top and implementation—enrollment, contributions, and benefits—within ordinary law.
3. Private Coverage, Reading Texts, And Why The Distinction Matters
Because constitutions secure rights rather than mandate private purchases, private markets typically operate as complements or alternatives within a regulated framework. Families may buy family health insurance to shorten wait times, access specialized networks, or add features like maternity, pediatric, or elder-care benefits, including parents health insurance focused on long-term support. Regulators set interoperability rules so health insurance plans for family coordinate with public benefits, benefit catalogs, and patient-rights standards. The result is a layered ecosystem in which public entitlements define a floor and general health insurance plans, where permitted, build optional ceilings. Equity goals, primary care focus, and social participation commonly influence payment methods and benefit design across both spheres.
Reading the underlying law works best through a simple sequence that ties constitutional promises to operational detail. 1) Spot rights-based wording: identify clauses recognizing the right to health or health protection and explicit State duties to organize, fund, or regulate services. 2) Link to implementing statutes: review the health or social security code for enrollment, contributions, and benefit packages—where mandates usually live. 3) Assess judicial influence: check major rulings on access, essential medicines, and financial protection. 4) Chart public–private touchpoints: see how private insurers, networks, and supplementary family plans are regulated alongside public entitlements. 5) Separate rights from buying duties: note that a right to health rarely equals a constitutional order to purchase coverage; purchase obligations are ordinarily statutory.
4. Policy Architecture And Divergent Models
Understanding this line prevents category errors that can derail reforms or contracts. Two countries can use nearly identical constitutional language yet diverge on enrollment rules, financing, and the balance between public provision and private policies because statutes and regulations do the heavy lifting. That is why family health insurance may flourish as a supplemental option in one jurisdiction yet remain limited in another, despite similar rights clauses. Moreover, the statutory locus of mandates enables incremental adjustments in contribution bands, targeted subsidies, and provider payment reforms without reopening constitutional debates, which preserves stability while allowing course corrections as utilization patterns, technology costs, and epidemiology change.
For decision-makers planning coverage expansions or benefit redesigns, the actionable path had been straightforward and legally durable. Draft reforms within ordinary law to fine-tune enrollment obligations, financing mixes, and benefit catalogs; use constitutional principles as a north star; and rely on judicial jurisprudence to maintain access standards and correct outliers. In parallel, regulate private offerings so general health insurance plans and health insurance plans for family align with patient-rights norms, data protections, and nondiscrimination rules. Taken together, these steps kept the system both adaptable and anchored, safeguarded universal aspirations, and signaled to households and markets that rights were guaranteed while purchase mandates, when chosen, were crafted and updated through statutes rather than constitutional fiat.