What if the standard paths of healthcare finance took an unexpected turn, leading hospitals into murky waters of legal challenges? Imagine a scenario where a patient, stuck in the intricate web of healthcare systems, faces both medical and legal implications after an accident. Such a case recently unfolded, impacting how hospitals and insurers interact in the realm of uninsured motorist (UM) funds.
Healthcare Financing in Unfamiliar Territory
The unexpected intertwining of healthcare billing practices and motorist insurance policies raises crucial questions about payment pathways for services rendered. When a hospital attempts to leverage resources typically reserved for accident victims to cover medical expenses, the matter shifts from routine finance to a confrontation of norms. This peculiar convergence paints a vivid picture of modern patients juggling both health and legal adversities. These events invite us to question the solidity of existing frameworks, as institutions grapple with balancing their financial operations and ethical responsibilities.
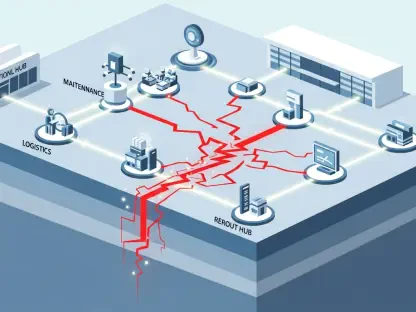
The Complex Tapestry of Financial Protocols
In this unfolding drama, hospital billing protocols and insurance coverage often sit at the crux of patient care and financial sustainability. The significance becomes clearer when examining the broader trends influencing how hospitals secure payments while navigating established mechanisms such as Medi-Cal. These traditional frameworks are vital, as they guarantee standardized procedures that protect both healthcare providers and patients. The adherence to these systems not only ensures transparency but also underpins a fair and accountable healthcare environment.
Unraveling Dameron Hospital’s Legal Conundrum
A significant legal confrontation emerged between Dameron Hospital Association and Progressive Casualty Insurance, a case centered around the attempt to bypass the usual Medi-Cal reimbursement. The hospital pursued direct compensation from a patient’s UM policy, diverging substantially from anticipated practices. Dameron’s actions, highlighted by specific claims of contract breaches and unfair practices, brought attention to unconventional maneuvers in hospital billing. This departure illuminates a broader issue, where attempts to exploit alternative payment structures can lead to convoluted legal battles and systemic disruption.
Judicial and Expert Opinions Shed Light
In dismissing Dameron’s claims, the court highlighted the misalignment of such demands with established insurance purposes, clarifying the role of UM coverage. This perspective draws attention to the critical distinction between compensation for individual losses and substituting standard hospital payments. Legal experts acknowledge that such judicial clarifications reinforce necessary boundaries, maintaining the integrity of insurance systems. Cases like these underscore a collective resolve to keep healthcare frameworks intact, safeguarding against unanticipated deviations that can skew the balance of care and finance.
Navigating the Road Ahead
The ruling prompts hospitals to rethink their strategies around insurance billing practices. Ensuring alignment with industry norms becomes crucial as institutions evaluate their approaches to mitigating complex claims. Strategies focusing on reinforcing policy compliance and maintaining transparent billing processes are now more pertinent than ever. This judicial decision also beckons policymakers and healthcare leaders to contemplate adjustments that further clarify financial responsibilities and promote sustainable practices. As hospitals adapt to these precedents, the emphasis remains on safeguarding the integrity of healthcare finance while ushering in informed, responsible change.