Imagine a scenario where an insurance giant like GEICO uncovers a multi-million-dollar fraud scheme, alleging that medical clinics in Florida have siphoned off $3.5 million through deceptive personal injury protection (PIP) claims, sparking intense debate across the insurance and legal sectors. This staggering accusation has raised critical questions about systemic fraud, regulatory oversight, and the innovative use of federal laws to combat such issues. This roundup dives into a collection of opinions, insights, and analyses from various industry perspectives to unpack the complexities of GEICO’s high-stakes lawsuit against two Florida clinics. The purpose here is to present a balanced view of the allegations, legal strategies, and broader implications for the auto insurance landscape in Florida, shedding light on whether such battles can reshape fraud enforcement.
Unpacking the Stakes: Fraud Allegations and Their Impact
The foundation of this legal clash rests on GEICO’s claims that two Florida clinics have engaged in a systematic fraud scheme for at least a few years, targeting auto accident victims covered by PIP policies. Industry observers note that the insurer’s lawsuit, filed in federal court, accuses the clinics of submitting thousands of false or inflated claims for services that were either unnecessary or never performed. This perspective emphasizes the financial toll, with losses exceeding $3.5 million, which ultimately burdens policyholders through higher premiums.
Contrasting views emerge from legal analysts who caution that while the monetary figure is striking, proving systemic fraud is a steep challenge. Some suggest that what GEICO labels as fraud might be interpreted by others as aggressive billing practices, a gray area at the intersection of healthcare and insurance. This debate highlights a critical tension: the need to protect insurers from exploitation versus ensuring medical providers aren’t unfairly targeted for legitimate, if ambitious, reimbursement strategies.
A third angle comes from consumer advocacy groups, who argue that the real victims are Florida drivers caught in the crossfire. Rising insurance costs due to fraudulent PIP claims have long been a pain point, and many in this camp stress that cases like this one expose deep flaws in the state’s no-fault insurance system. Their insights push for a broader discussion on how such legal battles might prompt much-needed reforms to safeguard policyholders.
Diving Deeper: Key Issues and Opinions on GEICO’s Lawsuit
Breaking Down the Alleged Multi-Year Fraud Scheme
At the heart of GEICO’s accusations lies a detailed narrative of deception, where the clinics reportedly billed for treatments by unqualified staff or for services that never occurred. Insurance fraud experts point out that such practices, if proven, represent a blatant abuse of the PIP system designed to support accident victims. The scale of the alleged scheme, involving thousands of claims, underscores the potential for widespread damage to trust in medical billing.
On the other hand, some healthcare industry commentators argue that the line between fraud and clerical error is often blurred. They suggest that what GEICO perceives as intentional deceit could stem from administrative oversights or misunderstandings of complex billing codes. This perspective urges caution in labeling entire operations as fraudulent without ironclad evidence of malicious intent.
A differing viewpoint from data analysts within the insurance sector highlights the importance of patterns in billing records. They note that anomalies, such as identical treatment plans for unrelated patients, often serve as red flags for investigators. This analytical lens supports GEICO’s stance, suggesting that the consistency of questionable practices over multiple years leans more toward deliberate fraud than mere coincidence.
Regulatory Violations and Legal Loopholes in Focus
GEICO’s complaint also zeros in on alleged breaches of Florida’s strict healthcare regulations, including misrepresentation of licensing and medical director compliance. Legal scholars familiar with state insurance laws emphasize that such violations, if substantiated, could significantly strengthen the insurer’s case. They argue that failing to meet regulatory standards isn’t just a technicality but a foundational issue that undermines the legitimacy of claims.
However, defense-oriented legal analysts counter that Florida’s PIP regulations are often vague or inconsistently enforced, creating loopholes that clinics might exploit without necessarily breaking the law. This opinion suggests that GEICO may struggle to prove intent, especially if the clinics argue they operated within ambiguous guidelines. The clash of interpretations here reveals a broader need for clearer statutes.
A regulatory perspective adds another layer, with some state officials and policy experts advocating for tighter oversight of PIP billing practices. They point out that cases like this expose systemic gaps, such as inadequate monitoring of medical director roles. Their input calls for proactive measures to close these loopholes, ensuring that legal battles don’t become the only recourse for insurers.
Leveraging RICO: A Bold Strategy Against Fraud
One of the most discussed aspects of this lawsuit is GEICO’s use of the federal RICO Act, typically associated with organized crime, to target alleged healthcare fraud. Insurance industry leaders view this as a groundbreaking move, reflecting a growing trend to apply heavy-hitting federal statutes against complex fraud networks. They believe a successful RICO claim could deter similar schemes across the state.
Skeptics within the legal community, however, warn of potential overreach. Some argue that applying RICO to civil disputes over medical billing risks diluting the law’s original purpose, potentially flooding courts with cases that stretch its scope. This concern raises questions about whether such a strategy might backfire, setting precedents that complicate rather than clarify fraud enforcement.
A middle-ground opinion from academic researchers in law and policy suggests that while RICO’s use is innovative, its success hinges on proving a coordinated, criminal enterprise. They note that if GEICO can establish a clear pattern of organized misconduct, this case could redefine how insurers combat fraud. This balanced take encourages watching the outcome closely for its impact on future legal tactics.
Kickbacks and Patient Exploitation: Ethical Concerns
Another contentious issue involves allegations of illegal referrals and kickback schemes, where patients were reportedly funneled into profit-driven treatment plans. Patient rights advocates express alarm over these claims, arguing that exploiting accident victims for financial gain is not only unethical but also erodes public trust in healthcare. Their stance bolsters GEICO’s moral argument in the case.
Conversely, some healthcare consultants suggest that referral arrangements are common and not inherently illegal, provided they prioritize patient care over profit. They caution against assuming malice in every coordinated treatment plan, urging a deeper look into whether patients genuinely suffered harm. This viewpoint challenges the severity of GEICO’s accusations, advocating for nuance.
Insights from past PIP fraud investigations in Florida, as shared by seasoned auditors, reveal that patient exploitation often serves as a powerful emotional and legal lever in such cases. They note that demonstrating harm to individuals can sway juries and regulators alike. This historical context indicates that if GEICO proves these claims, it could significantly tilt the case in its favor.
Critical Takeaways from the Debate
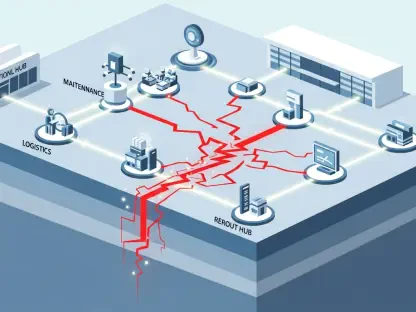
Synthesizing the diverse opinions, the scale of the alleged $3.5 million fraud stands out as a unifying concern, with most agreeing that PIP abuse remains a persistent problem in Florida. Insurance stakeholders stress the importance of advanced fraud detection tools, like data analytics, to flag suspicious billing patterns early. Their practical advice focuses on prevention as much as litigation.
From a regulatory standpoint, there’s a shared call for stricter PIP oversight, with suggestions ranging from mandatory audits of high-volume clinics to clearer licensing rules. These actionable ideas aim to address systemic vulnerabilities that allow fraud to flourish. The consensus here leans toward collaborative efforts between insurers and state authorities.
For consumers and industry watchers, staying informed is key. Engaging with local policy discussions or supporting advocacy for stronger protections can amplify the impact of cases like this. These steps empower individuals to contribute to a fairer insurance system while keeping abreast of evolving legal and regulatory landscapes.
Reflecting on the Discussion
Looking back, the roundup of perspectives on GEICO’s legal fight against Florida clinics paints a multifaceted picture of fraud, law, and ethics. The clash of opinions—from insurers pushing for accountability to legal skeptics warning of overreach—reveals the complexity of tackling PIP fraud. Each viewpoint adds depth to the understanding of this $3.5 million dispute.
Moving forward, stakeholders should consider investing in technology-driven fraud prevention, such as machine learning models to detect billing anomalies. Simultaneously, advocating for legislative updates to seal regulatory gaps could prevent future schemes. These actionable steps offer a path toward balancing the interests of insurers, providers, and policyholders in Florida’s challenging PIP market.