Welcome to an insightful conversation with Simon Glairy, a renowned expert in insurance and Insurtech, with a deep focus on risk management and AI-driven risk assessment in the healthcare sector. With the recent passage of the Big Beautiful Bill, the US healthcare system faces unprecedented financial, workforce, and liability challenges. In this interview, Simon unpacks the complexities of this legislation, exploring its impact on providers, the growing risks for healthcare workers and patients, and the critical role of brokers in navigating this turbulent landscape. Join us as we delve into the strategies and solutions needed to address these pressing issues.
Can you start by explaining what the Big Beautiful Bill is and how it’s reshaping the US healthcare system?
Absolutely. The Big Beautiful Bill is a sweeping piece of legislation recently passed that introduces significant regulatory changes to the US healthcare system. It’s primarily aimed at restructuring funding streams, which means cuts to Medicare and Medicaid reimbursements, as well as reductions in academic research funding and new tariffs on medical equipment. These changes are putting immense financial pressure on healthcare providers, forcing them to rethink operational models. Beyond finances, the bill also tightens immigration rules, impacting the availability of international healthcare workers, and it leaves a fragmented approach to AI regulations in healthcare. Overall, it’s creating a perfect storm of challenges around funding, staffing, and risk exposure.
What are some of the key financial pressures healthcare providers are facing as a result of this bill?
The financial strain is hitting providers from multiple angles. The cuts to Medicare and Medicaid reimbursements are particularly brutal because these programs are lifelines for many hospitals and clinics, especially in underserved areas. Reduced payments mean thinner margins, and for some facilities, it’s a question of survival. On top of that, there are cuts to academic research funding, which impacts innovation and training programs that hospitals often rely on. Then you’ve got tariffs on medical equipment increasing costs for essential tools. Collectively, these pressures are pushing providers to make tough choices, like cutting staff or delaying investments in infrastructure, which only compounds other risks down the line.
How are workforce shortages becoming such a critical issue under this new legislation?
Workforce shortages are at the heart of the crisis this bill is exacerbating. Even before this legislation, the healthcare sector was grappling with staffing issues post-COVID, but now it’s worse. The financial cuts I mentioned often lead to layoffs or hiring freezes since labor costs make up over half of a hospital’s budget. Add to that the stricter immigration rules in the bill, which limit access to international healthcare workers who’ve historically filled critical gaps, and you’ve got a recipe for severe shortages. The result is overworked staff, longer wait times, and a real threat to patient safety as care quality suffers.
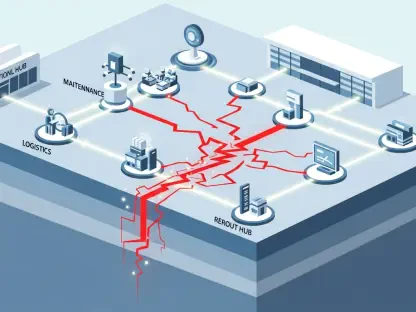
Can you walk us through the domino effect of these workforce shortages on healthcare workers themselves?
Certainly. When staff are stretched thin, it creates a vicious cycle. Overworked employees are more prone to physical injuries like musculoskeletal disorders from lifting patients or equipment, as well as slips and falls due to rushed movements. But the toll isn’t just physical—burnout is rampant. The mental health strain of doing more with less is leading to stress, anxiety, and depression, and in some states, these issues are now covered under workers’ compensation claims. This means not only are workers suffering, but providers are seeing a spike in claims, adding to their financial burden. It’s a feedback loop that’s hard to break without systemic change.
What strategies are healthcare organizations adopting to address these workforce challenges?
Many organizations are getting creative to cope. Some are redesigning roles so staff can work at the top of their licenses—meaning nurses and other professionals focus on patient care rather than administrative tasks. Technology is also playing a big role, with tools like automation reducing paperwork or streamlining scheduling to boost efficiency. But beyond efficiency, there’s a growing recognition that retention hinges on creating a safe, supportive environment. With workplace violence against healthcare workers on the rise since the pandemic, ensuring physical and psychological safety isn’t just nice to have—it’s essential. Providers who prioritize this are seeing better staff morale and lower turnover.
How are staffing shortages contributing to increased liability risks for healthcare providers?
Staffing shortages directly heighten the risk of errors in patient care. When there aren’t enough hands on deck, mistakes—like medication errors or missed diagnoses—become more likely. This is especially true in long-term care facilities, which rely heavily on Medicare funding and often operate with tight staffing ratios. These lapses in care can lead to serious harm, which in turn drives up professional liability claims against providers. It’s a cascading effect: fewer staff means lower quality care, which means more lawsuits, and ultimately higher costs for everyone involved. For providers, it’s a constant balancing act to manage these risks.
What advice would you give to brokers helping healthcare clients navigate the balance between risk retention and insurance coverage in this environment?
For brokers, the key is customization and education. Healthcare professional liability coverage is incredibly expensive right now due to the hard market and rising claims, so it’s critical to help clients find the sweet spot between retaining risk and transferring it through insurance. This means diving deep into a client’s specific exposures—whether it’s staffing issues or facility type—and designing coverage that matches those needs without overpaying. Brokers should also educate clients on proactive risk management, like investing in staff training or safety protocols, which can reduce claims over time. It’s about building resilience into their operations while ensuring they’re protected from catastrophic losses.
With the complexities introduced by AI in healthcare under this bill, how can brokers guide clients through the associated risks?
AI is a double-edged sword in healthcare right now, especially with the bill’s lack of unified federal regulation leaving a patchwork of state rules. Brokers need to help clients understand that while AI can drive efficiency in areas like hiring or workforce management, it also introduces risks like bias in data systems. If an AI tool inadvertently discriminates in hiring, it could lead to wrongful termination or discrimination claims. My advice is for brokers to encourage clients to develop clear digital roadmaps—strategies for AI adoption that prioritize ethics and compliance. Additionally, brokers should ensure clients have robust cyber and tech liability coverage to address these emerging risks.
What’s your forecast for the future of risk management in healthcare given the ongoing challenges with this legislation?
Looking ahead, I think risk management in healthcare will need to become even more proactive and integrated. The financial and workforce pressures from this bill aren’t going away anytime soon, and we’re likely to see more consolidation in the industry as smaller providers struggle to stay afloat. For risk management, this means a greater emphasis on data-driven strategies—using analytics to predict and mitigate risks before they spiral. I also foresee AI playing a bigger role, but only if ethical frameworks catch up to technology. Ultimately, the organizations that survive will be those that balance compassion with strategy, ensuring they care for their workers and patients while staying financially viable. It’s a tall order, but it’s the direction we’re heading.