In the intricate landscape of modern healthcare, a pressing issue looms large over hospitals and patients alike: the cumbersome and often detrimental process of prior authorization by commercial health insurers. This administrative hurdle, designed to control costs, frequently results in significant delays in treatment, leaving patients stranded in critical moments and pushing clinicians to the brink of burnout. The American Hospital Association (AHA) has taken a firm stand against these practices, advocating for immediate reform to safeguard patient care and alleviate the overwhelming burden on healthcare providers. As stories of delayed surgeries and abandoned treatments surface with alarming regularity, the urgency for systemic change becomes undeniable. This article delves into the core challenges posed by prior authorization, explores the proposed solutions, and examines the broader implications for the healthcare industry.
Addressing the Core Challenges
Unraveling the Impact on Patient Care
The prior authorization process, intended as a gatekeeping mechanism by insurers, often transforms into a barrier that jeopardizes patient health outcomes. Patients awaiting critical procedures or medications frequently face delays that stretch days or even weeks, leading to worsening conditions or, in extreme cases, treatment abandonment. Such interruptions not only undermine trust in the healthcare system but also place undue stress on families grappling with uncertainty. The AHA has highlighted how these delays can escalate into life-threatening situations, particularly for those with chronic or acute conditions requiring timely intervention. Beyond the immediate health risks, the psychological toll on patients navigating this maze of approvals cannot be overstated, as hope often gives way to frustration and despair in the face of bureaucratic inertia.
Straining the Healthcare Workforce
Beyond the direct impact on patients, prior authorization places an immense administrative burden on healthcare providers, contributing significantly to clinician burnout. Doctors and nurses spend countless hours filling out forms and appealing denials, time that could be better spent delivering care. This relentless paperwork exacerbates workforce shortages by reducing job satisfaction and diverting focus from patient interaction to bureaucratic tasks. The AHA notes that the resulting stress has even been linked to heightened workplace tensions, occasionally manifesting as violence against medical staff. As providers grapple with these challenges, the quality of care inevitably suffers, creating a vicious cycle that harms both the workforce and the individuals they serve. Addressing this issue is not merely about efficiency but about preserving the very foundation of compassionate healthcare delivery.
Pathways to Meaningful Reform
Industry Commitments and Regulatory Oversight
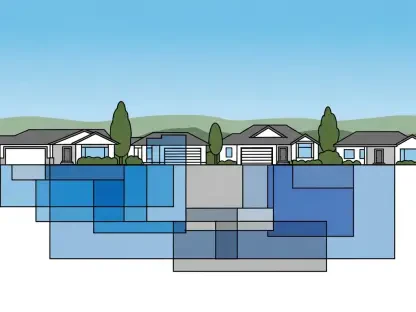
A glimmer of hope emerges from recent industry pledges facilitated by federal administration efforts, where major health insurers have committed to standardizing and reducing the volume of prior authorizations. This initiative targets plans across Medicare Advantage, Medicaid managed care, Health Insurance Marketplace, and commercial sectors, aiming to minimize delays in care delivery. The AHA has endorsed this move, viewing it as a critical step toward dismantling unnecessary obstacles to treatment. To ensure these promises translate into action, recommendations have been submitted to the Department of Health and Human Services and the Centers for Medicare & Medicaid Services, urging strict monitoring of insurer compliance with existing regulations. Such oversight is vital to hold insurers accountable and prevent backsliding on commitments that could otherwise remain mere rhetoric in the face of entrenched practices.
Legislative Efforts and Policy Opposition
On the legislative front, bipartisan support for the Improving Seniors’ Timely Access to Care Act (H.R. 3514/S. 1816) offers a promising avenue for streamlining prior authorization within Medicare Advantage. By reducing complexity and promoting uniformity, this bill seeks to alleviate the frustration caused by inconsistent authorization methods, benefiting both patients and providers. Meanwhile, opposition to specific insurer policies, such as Aetna’s proposed “level of severity inpatient payment” policy, underscores the need for vigilance. This policy, which would allow unilateral reimbursement reductions, threatens transparency and hospital viability, prompting strong resistance from the AHA. These combined efforts—legislative advocacy and policy critique—reflect a multifaceted approach to reforming a system that too often prioritizes profit over patient well-being, highlighting the necessity for sustained pressure on insurers to align with ethical standards.
Building a Future of Accountability
Reflecting on Past Advocacy Efforts
Looking back, the tireless advocacy by the AHA and other stakeholders painted a vivid picture of frustration with prior authorization delays and insurer policies that undermined care quality. Campaigns to expose these systemic flaws brought to light countless stories of patients caught in administrative limbo and providers stretched thin by paperwork. Efforts to collaborate with federal agencies ensured that the voices of those most affected were heard, while opposition to detrimental policies like reduced reimbursements challenged the status quo. This persistent push for change laid the groundwork for the industry pledges and legislative proposals that emerged as potential solutions, demonstrating that sustained pressure could shift the needle even in a complex healthcare landscape.
Charting the Next Steps for Systemic Change
Moving forward, the focus must shift to actionable strategies that cement these hard-won gains. Continuous monitoring of insurer compliance with reform pledges remains paramount, alongside robust enforcement of regulations by federal bodies. Hospitals and advocacy groups should deepen partnerships to amplify their influence, ensuring that patient-centered care drives policy decisions. Additionally, educating lawmakers on the real-world impacts of prior authorization can sustain momentum for bills aimed at simplification. As the healthcare community navigates this evolving terrain, the ultimate goal is clear: to transform a flawed system into one where medical professionals, not insurers, steer the course of patient care, fostering an environment of trust and efficiency for all involved.