When considering the escalating costs of healthcare, one startling disparity often catches attention: the significant price difference for the same medical procedures depending on where they are performed, which raises urgent questions about fairness and efficiency. Recent research has uncovered that commercial insurers pay substantially more for treatments conducted in hospital outpatient departments compared to ambulatory surgical centers, with an average difference of nearly 78% per procedure. This gap, amounting to thousands of dollars annually for insurers and patients alike, raises critical questions about the structure of healthcare pricing and the factors driving such disparities. As the debate over healthcare costs intensifies, understanding the reasons behind these differences becomes essential for stakeholders aiming to curb spending while maintaining access to quality care. This article delves into the nuances of site-based payment differentials, exploring the systemic and market-driven reasons for higher hospital costs and the potential pathways to address them.
Unpacking the Cost Disparity
Examining the Price Gap Between Facilities
A deep dive into recent data reveals a striking contrast in pricing for common medical procedures based on the setting in which they are performed. Hospital outpatient departments consistently charge commercial insurers far more than ambulatory surgical centers for identical services, with the average cost difference hovering around $1,489 per procedure across a range of treatments. This discrepancy mirrors patterns seen in government programs like Medicare, though the absolute dollar gaps differ due to varying baseline rates. Among major insurers, the variation is notable, with some managing to negotiate lower rates by limiting contracts with high-cost hospital facilities, while others face steeper expenses due to broader network requirements. This pricing dynamic not only burdens insurers but also trickles down to employers and patients, inflating overall healthcare spending in ways that demand closer scrutiny.
Market Dynamics Driving Higher Hospital Costs
Beyond the raw numbers, the reasons for elevated hospital costs lie in complex market dynamics and contracting practices. Hospitals often justify higher prices by pointing to their broader service offerings, including emergency care and specialized treatments that surgical centers typically do not provide. Additionally, larger insurers may prioritize extensive networks to meet the needs of diverse employer clients, resulting in agreements with higher-cost hospital departments. This strategic choice, while ensuring access, often comes at a premium that smaller or more selective insurers might avoid through targeted contracting. The tension between cost containment and network breadth creates a challenging landscape where savings are possible but not always prioritized, highlighting a systemic issue in how healthcare services are priced and negotiated across different facilities.
Pathways to Cost Reduction and Policy Reform
Leveraging Selective Contracting for Savings
One promising avenue for mitigating the high costs associated with hospital outpatient departments is through selective provider contracting, a strategy already employed by some insurers to notable effect. By focusing on partnerships with lower-cost facilities, certain companies have managed to reduce average procedure costs significantly, with potential savings estimated in the billions annually if adopted more widely. This approach, however, is not without hurdles, as it requires balancing cost efficiency with the need to maintain adequate access for patients across varied geographic regions. Insurers must navigate the risk of alienating employer clients who value comprehensive networks, making this a nuanced but viable option for curbing expenses. The success of such strategies underscores the importance of strategic negotiation in addressing the persistent price disparities between different healthcare settings.
Exploring the Role of Site-Neutral Payment Policies
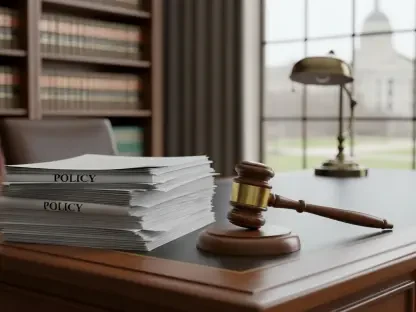
Another critical consideration in tackling cost disparities involves the potential implementation of site-neutral payment policies within the commercial insurance market. Such reforms, already a topic of debate in government healthcare programs, aim to standardize payments for procedures regardless of where they are performed, potentially saving substantial sums over time. However, opposition from hospital groups, who argue that higher payments are necessary to sustain their wide-ranging services, complicates the adoption of these policies. Additionally, the unique competitive dynamics of the commercial market mean that any policy changes must be carefully tailored to avoid disrupting existing insurer-provider relationships. Transparency and access to information for employers and patients also emerge as key concerns, suggesting that regulatory oversight might play a role in ensuring equitable pricing.
Reflecting on Past Challenges and Future Steps
Looking back, the persistent gap between hospital and surgical center costs has long challenged insurers, policymakers, and patients, with billions spent unnecessarily due to entrenched pricing differences. The resistance to change from certain stakeholders, coupled with the complexity of market-driven healthcare systems, has often stalled progress toward meaningful reform. Despite these obstacles, the evidence of potential savings through selective contracting and policy adjustments provides a clear signal for action. Moving forward, stakeholders must prioritize transparent data sharing to empower informed decision-making among employers and patients. Additionally, fostering dialogue between insurers, providers, and regulators could pave the way for balanced solutions that address both cost and access. As the healthcare landscape evolves, these steps offer a roadmap to reduce disparities and build a more sustainable system for all involved.