In the heart of Vermont, where rolling hills meet the harsh realities of a deepening health care affordability crisis, the annual budget hearings for 14 hospitals have captured widespread attention, marking a critical juncture for a state burdened by the nation’s highest health insurance premiums. Overseen by the Green Mountain Care Board, the state’s key health care regulator, these discussions for fiscal year 2026 wrapped up on August 5. With major insurers like Blue Cross Blue Shield of Vermont and MVP teetering on unstable financial ground, the stakes couldn’t be higher. These budget decisions don’t just crunch numbers—they directly shape the cost of medical services and determine how much Vermonters will pay for coverage, potentially altering access to essential care for countless families across the state.
The gravity of the situation is palpable, as soaring health care costs translate into real struggles for residents. Many find themselves caught between rising premiums and the fear of being priced out of necessary treatments. Vermont’s Chief Health Care Advocate, Mike Fisher, has pointed out that this crisis extends beyond hospital walls, intertwining with insurer challenges and systemic pricing issues. The outcomes of these hearings are poised to ripple through communities, influencing whether individuals can afford the care they need to maintain their health and well-being.
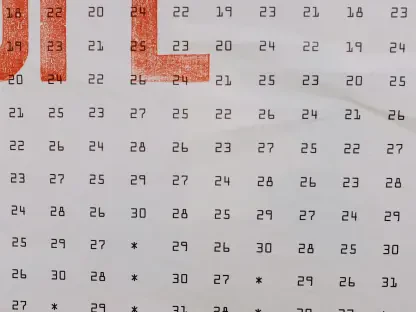
Hospital Budget Trends for 2026
Compliance with Regulatory Guidelines
A notable shift has surfaced in this year’s hospital budget proposals, setting them apart from the more aggressive requests of the past two fiscal cycles. The Green Mountain Care Board laid out stringent benchmarks for 2026, capping net patient revenue increases at 3.5%, operational expense growth at 3%, and commercial insurer charges at 3%. In a marked departure from previous trends, the majority of hospitals have either met or fallen below these targets, reflecting a heightened sensitivity to the affordability crisis gripping the state. For instance, Rutland Regional Medical Center, a prominent community hospital, proposed a decrease in net patient revenue by 1.7% and a reduction in commercial charges by 3.7%, while maintaining operational expense growth at a modest 2.8%. This trend suggests hospital leaders are prioritizing cost containment to ease the burden on Vermonters struggling with insurance costs.
This pattern of compliance isn’t limited to a single facility but extends across several larger hospitals, underscoring a collective effort to align with regulatory expectations. Institutions like Northwestern Medical Center and Southwestern Vermont Medical Center have similarly tabled proposals that either match or undercut the board’s guidelines, balancing their financial needs with public affordability concerns. Such restraint indicates a broader acknowledgment of the economic pressures facing residents, as well as a strategic response to the scrutiny of regulators. While these moderate budgets offer a glimmer of relief, they also raise questions about the long-term sustainability of hospital operations under such tight constraints, especially as demand for services continues to grow in an aging population.
Exceptions Among Critical Access Hospitals
Not all hospitals, however, have adhered to the Green Mountain Care Board’s stringent limits, particularly among smaller, rural facilities designated as critical access hospitals. These institutions, vital to remote communities, often face unique financial challenges due to lower patient volumes and higher per-unit costs. Springfield Hospital, for example, has requested an 8.3% increase in net patient revenue and a substantial 10% rise in operating expenses, far exceeding the board’s benchmarks. Similarly, Mt. Ascutney Hospital & Health Center and Copley Hospital have proposed hikes in certain budget categories, driven by the need to maintain essential services in areas with limited health care options. These exceptions highlight the distinct pressures smaller hospitals endure, which differ significantly from their larger counterparts.
Despite these outliers, some critical access hospitals have shown fiscal restraint, aligning more closely with regulatory expectations. Gifford Medical Center stands out by proposing no change in operating expenses and even a slight decrease in net patient revenue, demonstrating that moderation is possible even under challenging circumstances. This contrast among rural facilities reveals a complex landscape where financial survival often clashes with affordability goals. The Green Mountain Care Board faces the delicate task of weighing these unique needs against the broader imperative to control costs, ensuring that rural communities are not left without critical care while still addressing statewide economic concerns.
Legislative Impacts on Hospital Finances
New Laws and Revenue Cuts
Significant legislative changes are reshaping the financial outlook for Vermont’s hospitals, adding another layer of complexity to the budget hearings. A new state law, set to take effect on January 1, 2026, imposes caps on the prices hospitals can charge private insurers for specific outpatient pharmaceuticals, particularly injectable and IV-administered drugs used in treatments like immunotherapy and cancer care. This policy is projected to reduce collective hospital revenue by approximately $100 million, with the University of Vermont Medical Center (UVMMC) bearing the largest impact at an estimated $70 million loss. This substantial hit to income underscores how state interventions can directly alter hospital finances, potentially forcing adjustments in service delivery or staffing to offset the shortfall.
Beyond this specific measure, broader cost-control initiatives are under consideration, though their implementation remains uncertain. Discussions around reference-based pricing and proposals to cap commercial pricing for all hospital services at 500% of the Medicare rate signal a growing political resolve to tackle escalating health care costs. These potential reforms aim to create a more predictable pricing structure, but they also introduce new challenges for hospitals already navigating tight budgets. The interplay between legislative action and hospital revenue streams illustrates a critical tension: while intended to protect consumers, such policies may strain the ability of medical facilities to maintain quality care, particularly for complex treatments requiring significant investment.
Financial Pressures and Adaptation Strategies
The revenue cuts from legislative measures are pushing hospitals to rethink their operational models in profound ways. For UVMMC, the projected $70 million loss from drug price caps is not merely a budgetary line item but a catalyst for reevaluating resource allocation. Some facilities are already exploring cost-saving measures, such as streamlining administrative processes or renegotiating supplier contracts, to mitigate the impact. However, these adaptations often come with trade-offs, potentially affecting the scope of services offered or the speed of care delivery. The challenge lies in ensuring that financial adjustments do not compromise patient outcomes, especially in a state where access to specialized care can be limited outside urban centers.
Hospitals are also grappling with how to communicate these financial pressures to the public and regulators without fueling further concern. The risk of reduced revenue translating into diminished community trust looms large, as residents may worry about the availability of critical treatments. Moreover, the legislative push for cost control could set a precedent for additional restrictions, prompting hospital administrators to proactively seek alternative funding sources or partnerships. As these facilities adapt to a shifting policy landscape, the broader question remains whether such changes will achieve the intended balance between affordability and the sustainability of health care infrastructure in Vermont.
Stakeholder Perspectives and Systemic Challenges
Balancing Hospital Needs and Affordability
The budget hearings have brought to light a fundamental tension between maintaining hospital viability and ensuring health care remains affordable for Vermonters. Hospital leaders, represented by figures like Michael Del Trecco, president and CEO of the Vermont Association of Hospitals and Health Systems, have cautioned that while budgets are being kept lean, further reductions could jeopardize their capacity to meet community needs. Del Trecco has emphasized the importance of funding for transformative care delivery, arguing that overly restrictive budgets risk undermining long-term improvements. This perspective highlights the delicate balance hospitals must strike between fiscal restraint and the imperative to provide comprehensive services, especially in a state with diverse health care demands.
On the other side of the equation, the Green Mountain Care Board remains steadfast in its mission to protect consumers by enforcing tight budget limits. This regulatory focus is evident in recent cost-cutting realities, such as layoffs at UVMMC, which illustrate the tangible impact of financial constraints on hospital operations. These measures, while aimed at aligning with affordability goals, often stir public concern about potential declines in care quality or access. The board’s upcoming decisions on insurance rate requests, scheduled for August 22, will further test this balance, as they directly influence how much residents pay for coverage and how hospitals can fund their services.
Long-Term Solutions Over Short-Term Fixes
Amid the immediate focus on budget numbers, a consensus is emerging among stakeholders about the need for sustainable solutions to Vermont’s health care cost crisis. Advocates like Mike Fisher stress that affordability is a systemic issue, involving not just hospitals but insurers and pricing structures across the industry. Short-term cuts or caps, while offering temporary relief, fail to address underlying challenges such as rising demand for services and the high cost of medical technology. Fisher and others advocate for collaborative approaches that prioritize innovation, such as reimagining payment models to reward value over volume, ensuring that cost control doesn’t come at the expense of patient care.
The urgency for long-term strategies is underscored by the looming deadline for the Green Mountain Care Board to finalize hospital budgets by September 15. These decisions will have a cascading effect on insurance premiums, access to care, and the financial health of medical facilities. While the current trend of budget moderation offers some hope, it’s clear that more comprehensive reforms are needed to build a resilient health care system. Stakeholders across the spectrum agree that moving beyond reactive measures to proactive, sustainable frameworks is essential for ensuring that Vermonters can access affordable, high-quality care in the years ahead.
Reflecting on Broader Implications
Looking back on the 2026 budget hearings, it’s evident that Vermont’s hospitals took a measured approach, with most aligning with regulatory guidelines amid an unprecedented affordability crisis. The compliance of larger facilities and the struggles of critical access hospitals painted a nuanced picture of a state striving for balance. Legislative interventions, notably the cap on outpatient drug prices, introduced significant revenue challenges, particularly for major players like UVMMC. As the Green Mountain Care Board finalized its decisions, the focus shifted to actionable next steps. Hospitals must now explore innovative funding and operational models to adapt to reduced revenues without sacrificing care quality. Policymakers should prioritize developing sustainable payment systems that address systemic cost drivers, while regulators and advocates collaborate on reforms that protect both access and affordability. These efforts, if pursued with diligence, could pave the way for a more equitable health care future in Vermont.