Over four million Texans who depend on the Affordable Care Act (ACA) Marketplace for their health insurance are confronting a financial precipice that threatens their access to essential medical care. The central issue is the scheduled expiration of the Enhanced Premium Tax Credits at the end of the year, a federal policy change that is projected to cause insurance premiums to more than double for the majority of enrollees in 2026. These federal subsidies, first introduced in 2021, have been instrumental in making comprehensive health plans affordable for individuals and families across the state. Their termination is poised to create profound uncertainty, forcing people into exceedingly difficult decisions about their health and finances. This impending crisis unfolds in a state that already holds the unfortunate distinction of having the highest uninsured rate in the United States, raising serious concerns among health advocates and market experts about the far-reaching consequences for both individual well-being and the stability of the broader health care system.
The Human Cost of a Policy Cliff
The abstract numbers and policy debates surrounding the subsidy expiration find a poignant, real-world voice in the story of Shanice Jordan, a Dallas resident who was diagnosed with two types of lupus in 2003. Her experience serves as a stark reminder of the precariousness of the American health care system before the ACA. After aging out of her father’s insurance, her family struggled to afford the exorbitant cost of COBRA coverage, which reached an unsustainable $600 per month. They were eventually forced to make the difficult choice to go without insurance while her lupus was in remission, a decision that proved financially catastrophic when a subsequent flare-up resulted in a five-digit hospital bill they were unable to pay. For the Jordan family and countless others with preexisting conditions, the passage of the ACA in 2010 represented a long-awaited safety net, a promise of stability and access to care that had previously been out of reach for so many.
Today, the ACA marketplace allows Jordan to maintain a dedicated team of medical providers who are essential for managing her chronic autoimmune disease, but the impending subsidy expiration threatens to dismantle this carefully constructed support system. Her current monthly premium of $173 is set to skyrocket to an astonishing $942 for the exact same plan, an increase of more than 500%. This potential financial burden forces her to contemplate agonizing choices, such as whether to ignore potentially life-threatening pain simply to avoid accumulating insurmountable medical bills. She vividly recalls past emergencies where doctors informed her that waiting even one more day to seek treatment could have been fatal, a memory that underscores the life-or-death nature of her current dilemma. While she has considered switching to a lower-cost plan to mitigate the financial blow, she rightly fears losing access to the specific network of doctors, specialized services, and crucial medications that are indispensable for managing her complex condition.
A Statewide Crisis in the Making
The profound anxiety felt by Shanice Jordan is not an isolated case but rather reflects a growing sentiment of distress across Texas. Lynn Cowles, an advocacy volunteer with the public policy organization Every Texan, reports observing widespread “hesitance, confusion, a lot of disappointment, sometimes anger” among the many people she assists with ACA enrollment. She frames the dire situation as a choice between “two devastating financial situations”: either committing to potentially unmanageable annual premiums that could reach $20,000 for a family, or risking hundreds of thousands of dollars in medical debt from an unexpected health crisis. This impossible dilemma is forcing some families to make harrowing decisions, such as insuring only certain members of the household, which creates what are known as “mixed insurance status households,” or forgoing insurance altogether. This dangerous trend is widely expected to exacerbate Texas’s already critical uninsured rate, unraveling years of hard-won progress.
The looming premium hikes are creating a ripple effect of instability that threatens to undermine the very foundation of health security for millions. As families are pushed toward desperate measures to cope with rising costs, the collective impact will be felt far beyond individual households. The potential for a significant increase in the number of uninsured residents will place additional strain on community health resources and emergency services, which are already stretched thin. Moreover, the decision to forgo or limit coverage can have long-term consequences for public health, as preventable conditions may go untreated, leading to more severe and costly health outcomes down the line. Health advocates warn that without immediate legislative intervention to extend the subsidies, the state is on a path toward a public health crisis that will reverse the significant gains in coverage achieved over the past several years, leaving the most vulnerable populations exposed.
Destabilizing the Entire Health Care Market
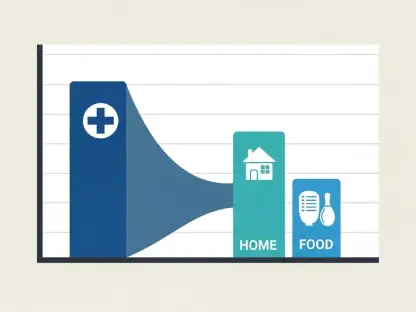
The consequences of the subsidy expiration extend well beyond the financial hardship of individual households, posing a significant threat to the stability of the entire health insurance market in Texas. Blake Hudson of the Texas Association of Health Plans highlights the remarkable progress made in recent years, with ACA enrollment in the state growing from 1.1 million in 2020 to approximately four million in 2025. This growth has been crucial in creating a more balanced and functional insurance marketplace. However, Hudson fears that the sudden loss of subsidies will not only halt this positive momentum but will actively reverse it, triggering a cascade of negative effects. A functional insurance market depends on a diverse risk pool that includes a mix of both “high users” of health care—typically older or sicker individuals—and “low users,” who are often younger and healthier. This balance ensures that premiums remain relatively stable and affordable for everyone.
When insurance becomes prohibitively expensive, it is overwhelmingly the healthier, “low user” demographic that is most likely to drop their coverage, as they may perceive the immediate financial cost as outweighing the potential risk of a future medical event. This exodus of healthy enrollees leaves a risk pool that is disproportionately composed of sicker, more expensive individuals. This imbalance, in turn, drives up the cost of insurance for everyone who remains covered, creating a vicious negative feedback loop often referred to as a “death spiral.” Furthermore, a substantial rise in the uninsured population places a greater financial strain on the entire health care system. Hospitals and other providers are forced to absorb more uncompensated care costs, particularly in emergency rooms, which can lead to increased prices for all patients and, in some cases, a reduction in the availability of essential medical services for the entire community.
The Unraveling of a Fragile Safety Net
The crisis also exposes a fundamental “preventive care paradox” that undermines public health goals. While navigators like Lynn Cowles can direct uninsured individuals to community health clinics for essential preventive services like cancer screenings, this represents only a partial and often inadequate solution. If a routine screening uncovers a serious issue, the individual is still left without the financial means to afford the necessary follow-up treatment, such as surgery, chemotherapy, or specialist consultations. This reality fosters what Cowles describes as “large scale feelings of betrayal,” as people begin to question the very point of getting screened if they know they cannot afford the subsequent life-saving care. This sentiment not only discourages proactive health management but also deepens the sense of hopelessness among those caught in the coverage gap, creating a cycle of delayed care and poorer health outcomes that ultimately affects the entire community.
The fate of individuals like Shanice Jordan ultimately depended on the outcome of last-minute negotiations by federal lawmakers to extend the critical tax credits. As she faced the worst-case scenario of a $900-plus monthly premium, the immense anxiety surrounding her upcoming January appointments became a daily burden. The situation amplified a perspective she felt was often misunderstood: the ACA was never just a program for those with chronic illnesses. It had become a vital resource for a diverse population, including entrepreneurs and small business owners who relied on the marketplace to pursue their professional goals while maintaining essential health coverage for themselves and their families. The uncertainty that clouded its future represented a profound challenge to the health and financial security of a significant portion of the Texan population, leaving a lasting impact on their ability to plan for a healthy and stable future.