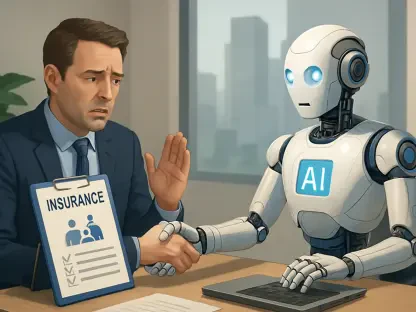
On December 23, 2024, President Biden signed into law two important pieces of legislation, the Paperwork Burden Reduction Act (Reduction Act) and the Employer Reporting Improvement Act (Reporting Act). Both acts target easing the administrative and reporting burdens on health plan sponsors and insurance providers under the Affordable Care Act (ACA). These legislative changes significantly alter how employers must handle ACA reporting, particularly when it comes to the distribution of Forms 1095-B and 1095-C, and offer more flexibility in responding to Internal Revenue Service (IRS) penalty assessments. The changes introduced by the new laws are expected to provide much-needed relief to employers grappling with the complexities of ACA compliance.
1. Ensure Timely Submission
Applicable large employers (ALEs) are still required to submit Forms 1094-C and 1095-C to the IRS by March 31, 2025, for electronic submissions, or by February 28, 2025, for paper submissions, pertaining to the coverage year of 2024. This requirement underscores the importance of timely and accurate reporting to remain in compliance with ACA regulations. The forms provide critical information regarding the health insurance coverage offered by the employer to their full-time employees and can be pivotal in determining whether the employer has satisfied its obligations under the ACA.
Ensuring timely filing involves several preparatory steps that employers must take well in advance of the deadlines. Employers should review their data collection and reporting processes to ensure that they can generate and submit the required forms accurately and punctually. With the Reduction Act and Reporting Act aiming to simplify the burden, employers may find this task somewhat less onerous, but it nonetheless remains a critical component of ACA compliance. Employers should also consider leveraging technology solutions that can streamline the form generation and submission process, thereby reducing the likelihood of errors and delays.
2. Implement Notice of Accessibility
Employers intending to benefit from the Reduction Act’s relief from automatic distribution must take certain steps to ensure that employees are informed of their rights. Before the IRS issues specific guidance on the matter, employers should begin preparing a “clear, conspicuous, and accessible notice” to inform employees that they can request a copy of Form 1095-C. This notice must be designed in a manner that ensures all employees are aware they can obtain the form upon request, thereby promoting transparency and accessibility.
While a model notice has not yet been released by the IRS, employers can draft a notice based on good faith efforts and existing best practices. The notice should be easily understandable and prominently displayed through various communication channels, such as email, internal websites, or physical postings in common areas. Employers should also establish procedures for handling and fulfilling requests for the forms promptly, ensuring compliance with the stipulated timeframes. By taking these proactive steps, employers can effectively implement the Reduction Act’s provisions and reduce their administrative burdens.
3. Consider State Requirements
Employers with employees in states that have individual health insurance mandates must remain aware of any state-specific requirements that may still necessitate the distribution of paper forms. States such as California, Massachusetts, New Jersey, Rhode Island, and Washington, D.C., have individual mandate requirements that could require employers to provide paper forms regardless of the federal Reduction Act’s provisions. Therefore, employers should not overlook the importance of state-level compliance when implementing the new ACA reporting changes.
To navigate these state requirements, employers should consult with their ACA vendors and legal advisors to determine the best approach to ensure compliance. This might involve maintaining parallel processes for federal and state reporting or leveraging technology solutions that cater to both sets of requirements seamlessly. Employers should also stay updated on any changes or updates to state mandates that could impact their reporting obligations. By adopting a comprehensive compliance strategy, employers can mitigate risks and avoid potential penalties associated with state-level reporting requirements.
4. Review Response Procedures for Penalty Notices
The Reporting Act extends the period during which employers can respond to IRS penalty notices from 30 days to 90 days. This significant change provides employers with additional time to review and address any potential ACA coverage failures, thereby mitigating the risk of incurring penalties. To take full advantage of this extended response window, employers must review and update their internal procedures for handling penalty notices, ensuring that they are prepared to effectively manage the additional time allowed.
Employers should familiarize themselves with the new response period and train their teams accordingly to ensure prompt and accurate responses to IRS penalty letters. This might involve designating a team or individual responsible for overseeing penalty notices, ensuring that all necessary documentation and information are readily available to support responses within the 90-day window. Additionally, employers should consider having a standard protocol for investigating and addressing any coverage failures identified in penalty notices, thereby reducing the likelihood of penalties escalating and impacting the organization’s financial health.
5. Monitor IRS Guidance
On December 23, 2024, President Biden enacted two pivotal pieces of legislation: the Paperwork Burden Reduction Act and the Employer Reporting Improvement Act. Aimed at alleviating the administrative and reporting load on health plan sponsors and insurance providers under the Affordable Care Act (ACA), these laws bring about significant changes in ACA reporting requirements. Specifically, they modify how employers must manage the distribution of Forms 1095-B and 1095-C, and they introduce greater flexibility for responding to Internal Revenue Service (IRS) penalty assessments. These updates are designed to offer crucial relief to employers who have been struggling with the intricate demands of ACA compliance. As a result, employers are expected to find the reporting process to be more streamlined and less cumbersome, aiding them in meeting their obligations more efficiently. The legislative changes symbolize a significant step toward making healthcare administration more manageable for businesses nationwide.