In the rapidly evolving landscape of medical innovation, gene therapies have emerged as a groundbreaking solution, offering the potential to cure conditions once deemed untreatable in the United States, symbolizing a new era of hope for countless patients. These therapies, meticulously evaluated and approved by the US Food and Drug Administration (FDA), represent a significant advancement for those battling severe genetic disorders. However, beneath this promise lies a troubling reality: not all patients can access these transformative treatments due to significant inconsistencies in commercial health plan coverage. While the FDA sets a benchmark for safety and efficacy, many insurers impose stricter criteria, creating a fragmented system where access often hinges on narrow eligibility requirements. This article delves into the critical gaps between regulatory approvals and insurance policies, examining how financial, clinical, and equity challenges shape patient outcomes. By exploring these disparities, a clearer picture emerges of the systemic barriers that must be addressed to ensure fair access to cutting-edge care.
Regulatory Approvals Versus Insurer Restrictions
The process of bringing gene therapies to market involves rigorous scrutiny by the FDA, which bases its approvals on extensive clinical trials demonstrating safety and efficacy for specific patient groups. These approvals often encompass broader indications, reflecting a comprehensive assessment of who might benefit from the treatment. Yet, commercial health plans frequently diverge from this framework, crafting coverage policies that adhere strictly to the parameters of pivotal trials. This conservative stance results in limited access, as only patients matching the exact trial demographics or clinical profiles qualify for coverage. Such restrictions mean that individuals who fall outside these narrow boundaries—despite being within the FDA’s approved scope—often face denials, leaving them without access to potentially life-altering therapies. This disconnect highlights a fundamental tension between regulatory science and payer decision-making, where the latter prioritizes certainty over inclusivity, often at the expense of patient needs.
Beyond the immediate impact on access, this misalignment between FDA guidelines and insurer policies creates a ripple effect across the healthcare system. Patients and providers must navigate a complex web of requirements, often spending significant time and resources to appeal denials or seek alternative funding. The burden of proof falls heavily on those seeking treatment, as insurers may demand additional documentation or prior authorizations that delay care. Moreover, this gap undermines the intent of regulatory approvals, which aim to ensure broad availability of safe and effective treatments. As gene therapies continue to advance, the persistence of such discrepancies raises questions about how well the healthcare system can adapt to innovation. Without closer alignment between regulators and payers, the full potential of these therapies risks remaining out of reach for many who stand to benefit, perpetuating a cycle of limited access and frustration.
Equity Challenges in Access to Innovative Treatments
One of the most pressing issues stemming from restrictive coverage policies is the exacerbation of healthcare disparities across diverse populations. Clinical trials for gene therapies often fail to include representative samples of racial minorities, elderly patients, or individuals with comorbidities due to historical and logistical barriers. When commercial health plans base coverage decisions on these trial data, they inadvertently exclude underrepresented groups who may not match the trial’s specific criteria but could still benefit under FDA indications. This creates a troubling inequity, where access to cutting-edge treatments becomes tied to demographic or clinical profiles rather than medical need. Such practices risk widening existing gaps in healthcare outcomes, particularly for communities already facing systemic barriers to care, and underscore the urgent need for more inclusive approaches to both research and coverage.
Addressing these equity concerns requires a multifaceted effort that extends beyond the scope of individual insurers. The lack of diversity in clinical trials is a well-documented challenge, often rooted in structural issues like limited outreach or access to research facilities in underserved areas. When coverage policies mirror these unrepresentative datasets, they perpetuate a cycle of exclusion that disadvantages vulnerable populations. For instance, older adults or those with multiple health conditions may be deemed ineligible despite potential benefits, simply because trial participants were younger or healthier. This raises ethical questions about fairness in the distribution of innovative care. Policymakers, researchers, and insurers must collaborate to diversify trial participation and develop coverage frameworks that account for real-world patient diversity, ensuring that gene therapies do not become a privilege reserved for a select few but a resource accessible to all in need.
Financial Pressures Shaping Coverage Decisions
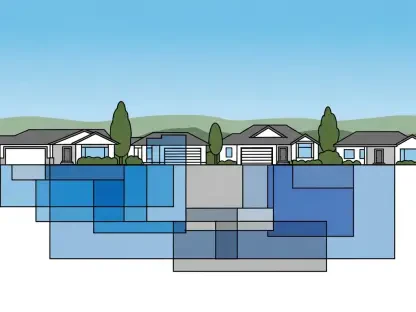
The staggering costs associated with gene therapies, often ranging from hundreds of thousands to millions of dollars per patient, play a central role in shaping insurer behavior. Commercial health plans, tasked with balancing budgets and patient care, adopt stringent criteria to manage financial risk, ensuring that coverage is extended only to those most likely to benefit as evidenced by trial outcomes. This cautious approach frequently involves additional hurdles such as extensive documentation, prior authorizations, or specific diagnostic requirements, all designed to justify the high expenditure. While these measures aim to align costs with therapeutic value, they often delay or deny access, leaving patients in limbo as they await approvals. The financial stakes of these treatments thus create a palpable tension, where the promise of long-term cures must be weighed against immediate budgetary constraints within the healthcare system.
This financial calculus extends beyond individual patient cases to influence broader payer strategies in the realm of innovative medicine. Insurers often grapple with uncertainties about the long-term effectiveness of gene therapies outside controlled trial settings, prompting a preference for conservative coverage policies. The upfront costs, while significant, are sometimes offset by the potential for reduced future medical expenses if a therapy proves curative. However, without robust data on real-world outcomes, payers remain hesitant to expand eligibility beyond trial parameters. This risk-averse mindset, while understandable from a fiscal perspective, can hinder the adoption of therapies that might benefit a wider population. As the field of gene therapy grows, finding mechanisms to share financial risk—such as value-based pricing or outcome-based reimbursement models—could help alleviate these pressures, enabling insurers to support broader access without compromising sustainability.
Navigating Variability in Coverage Policies
A significant challenge for patients and clinicians lies in the lack of uniformity among commercial health plan policies for gene therapies. Each insurer may establish distinct eligibility criteria, documentation needs, or appeal processes, resulting in a patchwork system that breeds confusion and unpredictability. For patients seeking treatment, this variability translates into uncertainty about whether coverage will be granted, often requiring extensive coordination with providers to navigate differing requirements. Clinicians, too, face administrative burdens as they attempt to align patient needs with disparate payer rules, diverting time from direct care. This lack of standardization not only complicates access but also erodes trust in the healthcare system, as patients struggle to understand why coverage decisions differ so widely across plans for the same FDA-approved therapies.
The call for greater transparency and consistency in coverage decision-making resonates as a potential solution to these challenges. Harmonizing policies to reflect evolving scientific evidence, rather than fragmented trial-based criteria, could simplify the process for all stakeholders. Transparent guidelines would provide clearer expectations, reducing the guesswork involved in seeking approvals and minimizing delays in treatment. Furthermore, standardized approaches could lessen the administrative load on healthcare providers, allowing them to focus on patient outcomes rather than paperwork. As gene therapies become more prevalent, establishing a more unified framework for coverage decisions will be essential to streamline access. Collaboration between regulators, insurers, and medical professionals to develop such guidelines could pave the way for a more equitable and efficient system, ensuring that patients face fewer barriers when pursuing life-changing treatments.
Future Pathways Through Real-World Evidence
Looking toward solutions, the integration of real-world evidence (RWE)—data derived from actual patient experiences after a therapy’s approval—holds immense potential to reshape coverage policies for gene therapies. Unlike initial trial data, which reflect controlled and often narrow settings, RWE offers insights into how treatments perform across diverse populations in everyday clinical practice. By incorporating this evidence, insurers could move beyond rigid trial-based criteria to develop more inclusive policies that account for a broader range of patient profiles. This shift could address current limitations in access, providing a more accurate picture of therapeutic benefits and risks in real-world scenarios. However, the adoption of RWE into payer frameworks remains slow, highlighting a gap between regulatory advancements and insurance practices that must be bridged to optimize patient care.
Policy innovation also plays a crucial role in paving the way for improved access to gene therapies. Encouraging dialogue among stakeholders—regulators, payers, clinicians, and patient advocates—can foster the development of dynamic coverage models that evolve with scientific progress. For instance, leveraging RWE might enable insurers to adjust eligibility criteria over time as more data becomes available, ensuring that policies remain relevant and fair. Additionally, exploring alternative reimbursement strategies, such as tying payments to patient outcomes, could mitigate financial concerns while expanding access. As the landscape of gene therapy continues to advance, prioritizing these forward-thinking approaches will be vital. By embracing real-world evidence and innovative policy solutions, the healthcare system can better balance the promise of cutting-edge treatments with the imperative of equitable access, ultimately benefiting a wider array of patients in need.
Bridging Gaps for a Fairer Healthcare Future
Reflecting on the challenges faced, it becomes evident that commercial health plans have often prioritized stringent criteria over the broader FDA indications for gene therapies, driven by both clinical caution and financial constraints. This approach, while offering some safeguards, restricts access for many patients and deepens equity concerns, particularly for underrepresented groups. Variability in policies across insurers further complicates the landscape, creating uncertainty and delays in care. Yet, amidst these hurdles, a path forward emerges through past discussions on real-world evidence and policy reform. Moving ahead, stakeholders must focus on integrating such evidence to craft inclusive coverage frameworks, while innovative reimbursement models could ease financial tensions. Collaborative efforts to standardize and make decision-making transparent will be key to ensuring that the transformative potential of gene therapies is realized by all who need them, paving the way for a more just and sustainable healthcare system.