Imagine a scenario where millions of Americans battling cancer suddenly find themselves grappling with skyrocketing health care costs, unable to afford the treatments that keep them alive. This dire situation is becoming a reality for over 18 million individuals living with cancer as critical federal health care policies undergo significant changes. Starting next year, the expiration of marketplace premium tax credits, coupled with new regulatory shifts, threatens to dismantle the fragile financial safety net that many patients rely on. With premiums poised to spike and out-of-pocket expenses climbing, access to life-saving care is at risk for a substantial portion of this vulnerable population. The urgency of the situation cannot be overstated, as these policy changes could redefine the landscape of health care affordability for those who need it most, pushing many into impossible choices between treatment and financial ruin.
Financial Barriers on the Horizon
As of January 1, 2026, premium tax credits for health care plans on HealthCare.gov are set to plummet by an average of 93 percent across numerous states, directly impacting 86 percent of cancer patients who depend on these subsidies. This drastic reduction will render essential services unaffordable for many, exacerbating an already challenging journey through illness. Beyond the credit cuts, a pending rule slated for next year will raise out-of-pocket cost-sharing limits for private insurance, adding another layer of financial strain. Additionally, the budget reconciliation law introduces mandatory annual re-enrollment for marketplace coverage, creating a risk of unintentional lapses for patients with complex conditions. Such lapses could interrupt critical care, particularly for those managing chronic cancers, where consistency is paramount. The convergence of these policy shifts paints a grim picture, threatening to erode access to affordable health care at a time when patients are least equipped to bear the burden of increased costs and bureaucratic hurdles.
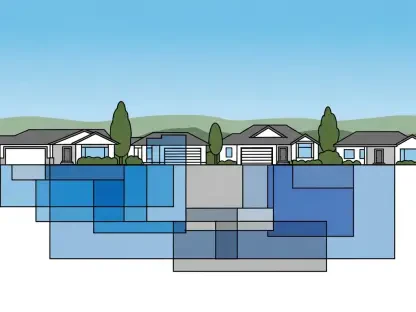
Regional Disparities and Vulnerable Demographics
A deeper analysis reveals that the impact of these changes is not uniform, with regions boasting higher-than-average cancer rates facing steeper premium hikes—up to 20 percent more than areas with lower rates. In twelve states, this translates to over $1,000 in additional annual costs for cancer patients in affected counties, with states like Alaska, Wyoming, and West Virginia bracing for the highest dollar increases. Meanwhile, places like Delaware, Indiana, Kansas, and New Hampshire, where all residents live in high-cancer-rate areas, face uniform barriers to affordable coverage. Older enrollees on HealthCare.gov in these regions are especially at risk, as the elimination of automatic re-enrollment—previously a safeguard—compounds their vulnerability. Premiums for this demographic are expected to rise faster than for younger individuals, heightening the chance of coverage loss. This stark disparity underscores how policy changes disproportionately burden specific communities and age groups, amplifying existing inequities in health care access.