Navigating the American healthcare system has become an increasingly complex and frustrating experience for millions, defined by opaque pricing, restrictive insurance networks, and the constant threat of surprise medical bills. In response to this widespread dissatisfaction, a fundamentally different approach is emerging, one that seeks to strip away the layers of bureaucracy and restore a direct connection between patient and doctor. This direct-pay model, championed by companies like UberDoc, is pioneering a transparent marketplace that operates almost entirely outside the traditional insurance-based framework. By positioning the patient as a direct consumer and the physician as an independent service provider, this market-driven alternative aims to bring simplicity, clarity, and affordability to an industry long overdue for disruption. The core premise is radical in its simplicity: what if patients knew the full cost of care upfront and could pay for it directly, just like any other service?
A New Philosophy for Patient Care
At the heart of the direct-pay movement lies a foundational commitment to absolute price transparency, a principle that directly confronts one of the most significant sources of patient anxiety. Within this model, physicians set a fixed, all-inclusive price for an appointment, which patients see and agree to before booking care. This simple mechanism completely eradicates the problem of surprise medical billing, empowering consumers with the certainty and control they have long been denied. This empowerment extends beyond just cost; it allows patients to bypass the gatekeeping of insurance referrals and the limitations of restrictive provider networks, granting them the freedom to choose any specialist they need. Simultaneously, the model restores a crucial degree of autonomy to physicians. By enabling them to set their own fees and manage their services without interference, it frees them from the administrative burdens and clinical constraints imposed by insurance payers, allowing them to focus their expertise on patient care.
This paradigm shift also necessitates a fundamental redefinition of the role of health insurance in the United States. Proponents of the direct-pay model argue that insurance has become a convoluted and inefficient intermediary for routine and preventative care, a function it was never designed to perform. Instead of advocating for the complete abolition of insurance, this approach suggests recalibrating its purpose. Insurance, in this view, should revert to its original function as a safety net for catastrophic, high-cost, and unexpected medical events, such as major surgeries or serious illnesses. For a significant portion of healthcare needs, including primary care visits and specialist consultations, patients are encouraged to take direct ownership of their health costs and outcomes. This separation of responsibilities aims to make everyday healthcare more affordable and accessible while ensuring that a robust insurance system remains in place to protect individuals from financial ruin in the face of a true medical crisis.
Making Direct Pay a Practical Reality
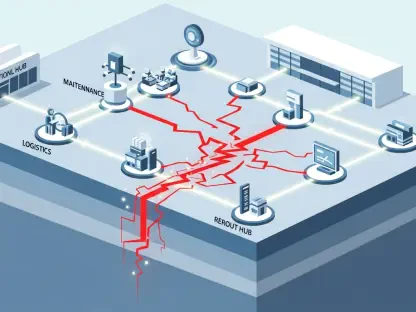
The operational framework for this new model is a pragmatic hybrid, skillfully blending the convenience of modern digital health with the enduring necessity of traditional, in-person medicine. Recognizing that a physical examination remains the gold standard for many diagnoses, the vast majority of appointments facilitated through this system are for face-to-face consultations. The platform ingeniously leverages the existing brick-and-mortar offices of its participating physicians, who are geographically dispersed across 44 states. This strategy creates an extensive, asset-light network without the immense capital expenditure required to build new facilities. Complementing this physical presence, virtual care accounts for approximately a quarter of all appointments, serving as a vital tool to bridge geographic gaps, provide care in underserved areas, and offer a convenient option for follow-ups and consultations that do not require a physical presence, thus ensuring comprehensive and flexible access.
To ensure its sustainability and growth, the business strategy relies on a multi-faceted revenue model that deliberately avoids imposing subscription or membership fees on patients. This is a key differentiator in a market increasingly populated by concierge and membership-based platforms. Patients pay only for the specific care they need on a per-appointment basis, using a credit card or a Health Savings Account (HSA) for a simple, one-time transaction. Beyond this core transactional revenue, two other significant income channels have been established to create a stable financial foundation. The first is a physician-focused Software-as-a-Service (SaaS) model, where board-certified specialists can subscribe to a suite of software tools to manage their practice. The second is a business-to-business (B2B) approach, involving contracts with self-funded employers who pay a per-member-per-month (PMPM) fee, offering the direct-pay service as a valuable and cost-effective employee health benefit.
The Future of Direct Pay Tech and Expansion
Looking toward the future, the integration of advanced technology is set to significantly enhance the direct-pay model, with a suite of Artificial Intelligence products planned for a 2026 launch. This AI strategy is two-pronged, designed to benefit both physicians and patients. For clinicians, AI tools will be developed to drastically reduce the administrative burden that consumes a large portion of their time and resources. This includes streamlining the often-tedious processes of physician onboarding and credentialing, facilitating practice marketing to attract new patients, and ultimately lowering operational costs. For patients, AI will be deployed to create sophisticated navigation tools that help them identify the most appropriate specialist for their symptoms and needs. Critically, these tools will also allow patients to compare costs by showing an estimate of what their out-of-pocket expenses would be if they were to use their traditional insurance plan, providing a data-driven comparison that highlights the value of transparent pricing.
The company’s ambitious roadmap for growth was not limited to technological innovation; it also included a clear strategy for corporate expansion financed through public capital. Mergers and acquisitions were identified as a key component for accelerating this growth, with the company actively exploring strategic collaborations that would expand patient access, enhance its technology platform, and strengthen its overall value proposition. To fund this next phase, a plan was set in motion to tap into public equity markets. This involved an initial listing on Canadian public exchanges, with a subsequent move to the over-the-counter (OTC) exchange in the United States. This strategic approach signaled a bold intention to scale the direct-pay model, positioning it not as a niche alternative but as a formidable competitor in the national healthcare landscape, particularly as consumers continued to seek more affordable and transparent options.